Anti-Aging Supplement May Rejuvenate Healthy And Osteoarthritic Human Joint Cells
The NAD+ boosting compound Urolithin A also helped osteoarthritic mice with cartilage breakdown, swollen joints, and pain. This suggests that Mitopure could help joints work and move better as people age or get sick.
Highlights:
- Dysfunction of the cell’s energy-producing centers (mitochondria) is a hallmark of joint aging and osteoarthritis.
- Urolithin A improves mitochondrial function in human cartilage cells from healthy donors and osteoporosis patients.
- In a mouse model of osteoporosis, Urolithin A improves joint mitochondrial health, reduces inflammation, and protects against osteoporosis-associated cartilage degeneration and pain.
According to a study done by the Swiss life science company Amazentis and Scripps Research, Urolithin A “energized” cartilage-forming cells (called chondrocytes) from the joints of both healthy humans and patients with osteoporosis, a common condition in which bones become weak and brittle, usually as we age. Also, in a mouse model, Urolithin A, a postbiotic that has been shown to give cells energy by improving mitochondrial health, slowed the progression of osteoporosis, cartilage degeneration, joint swelling, and pain. These findings imply that Urolithin A has the potential to improve mobility and aid in joint structural repair. The study was published in Aging Cell.

Compromised Cartilage Cells Cause Osteoarthritis
Osteoarthritis is the most common joint disease and a leading cause of disability in the western world. The main risk factor for getting osteoarthritis and having it get worse is getting older. Osteoarthritis is becoming more common as the human population ages, and it is expected to be one of the most common diseases in the next 10 years. Even so, there are no treatments for osteoarthritis that change the way the disease works, and the available drugs are only used to treat pain.
Chondrocytes are the only type of cell that can be found in mature cartilage. They are responsible for how the articular tissue works and stays together and in balance. These cartilage cells divide very slowly, which makes them more likely to get hurt over time. This makes their ability to reproduce and make new cells get worse over time, which increases the risk of osteoarthritis with age.
A Mess of Malfunctional Mitochondria
Mitochondrial dysfunction is a common feature of joints affected by osteoarthritis. Chondrocytes have a lower mitochondrial energy-generating capacity in osteoarthritis compared with healthy cartilage. The inability of joint cells to make new mitochondria through mitochondrial biogenesis is one thing that slows down mitochondrial metabolism. Also, chondrocytes in joints with disease have more mitochondria that don’t work because the cells aren’t able to remove damaged mitochondria through a process called mitophagy.
Mitophagy doesn’t function properly in many age-related diseases, and treatments to fix this problem have shown promise in conditions like muscle aging, heart disease, and neurodegeneration, among others. Targeting mitophagy is seen as a possible way to treat osteoarthritis that should be looked into. But while interventions have been tried to bring back mitochondrial biogenesis and boost mitochondrial respiration, no pharmacological method has yet been tested to bring back mitophagy in preclinical models of osteoarthritis.
Urolithin A Ups Mitochondrial Health in Human Cartilage Cells
Urolithin A is a metabolite that is made by the gut microbiome when certain foods, like pomegranates, berries, and nuts, are eaten. Urolithin A has a positive effect on muscle health in lab models of aging and in people. Studies have shown that Urolithin A slows down the aging of muscles in mice and increases the amount of nicotinamide adenine dinucleotide (NAD+), which is a key part of making energy. And in a randomized trial with middle-aged adults, it was shown that Urolithin A is safe for people and improves muscle strength, exercise performance, and biomarkers of mitochondrial health.
D’Amico and his team looked into how Urolithin A affects mitophagy and how mitochondria work in human knee joint cells from healthy donors and people with osteoarthritis. These experiments found that Urolithin A improves chondrocyte metabolic function by specifically activating mitochondrial energy production in both healthy and osteoarthritic subjects.
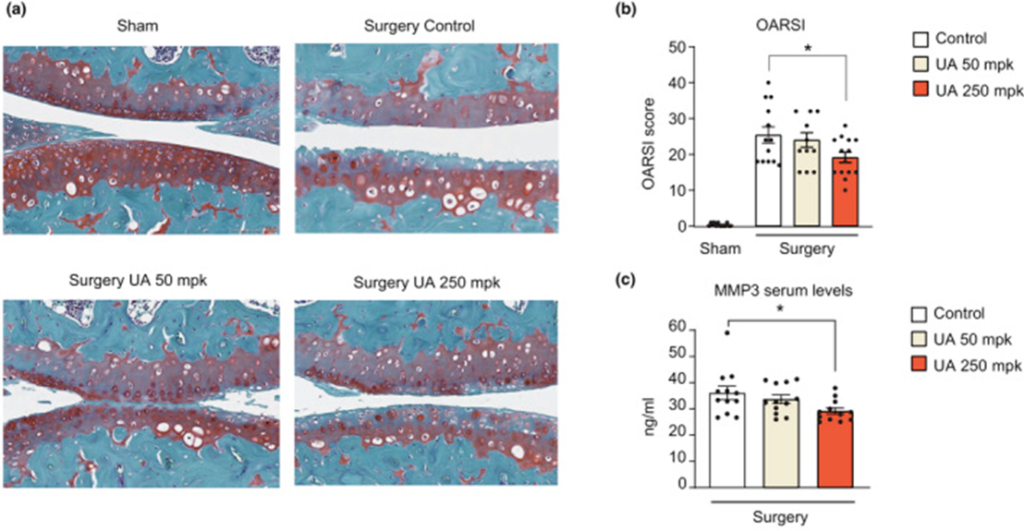
To see if these results were the same in whole animals, D’Amico and his team used a surgically-induced mouse model of osteoarthritis to test Urolithin A’s ability to stop cartilage from breaking down, stop inflammation, and relieve pain. Mice were given either a control diet or a diet with 50 or 250 mg/kg of Urolithin A added to it for 8 weeks after surgery. Following surgery, knee joints exhibited cartilage erosion in the femur and tibia, including loss of the cartilage lining of joints (the superficial zone). Urolithin A significantly reduced the OARSI score (lesion severity and percentage of the area affected in the entire knee) and circulating levels of metalloproteinase 3 (MMP3), a well-established blood biomarker associated with increased cartilage degradation, after 8 weeks of treatment. Also, higher doses or longer treatments could make Urolithin A even better at relieving pain.
To tie the human and mouse experiments together, the researchers looked at the effects of Urolithin A on mitochondrial health, measuring biomarkers of mitophagy and mitochondrial content in joint tissues of osteoarthritis mice. These experiments indicated that Urolithin A treatments could increase total mitochondrial content and the relative number of mitochondria undergoing mitophagy.
This work shows that Urolithin A has a positive effect on the health of mitochondria in joints and backs up the idea that Urolithin A could improve joint function and mobility in both healthy people and people with osteoarthritis. Researchers say that Urolithin A is the only compound that has been tested in preclinical models of osteoarthritis and could both reduce inflammation and improve the health of mitochondria. Because of this evidence and the fact that there aren’t any good drugs for osteoarthritis, more research needs to be done to see how Urolithin A affects osteoarthritis in clinical settings.
Model: Human primary chondrocytes; Mouse model of osteoarthritis
Dosage: 50 & 250 mg / kg Urolithin A (Mitopure)

