Eating Less Food 2 Days Per Week Reverses Diabetes, Outperforming Most Prescribed Anti-Diabetes Drug Metformin
5:2 intermittent fasting — limiting food intake for two nonconsecutive days of the week — improves blood sugar control in newly diagnosed diabetics, placing some into remission.
Highlights:
- 5:2 intermittent fasting improves blood sugar control more than the anti-diabetes pharmaceuticals metformin and empagliflozin.
- 5:2 intermittent fasting leads to significantly greater weight loss than metformin and empagliflozin.
Cancer, heart disease, and neurodegenerative disorders are more likely to develop in individuals with type 2 diabetes (T2D). Fortunately, T2D is one of the few chronic age-related conditions that can be reversed via dietary intervention. Moreover, purported T2D-reversal regimens like 5:2 intermittent fasting (5:2 IF) can potentially prevent T2D.
Scientists from the Chinese Academy of Medical Sciences have found that 5:2 IF improves aspects of T2D, including placing more people into remission, more than standard pharmaceutical interventions like metformin. What’s more, they found that 5:2 IF leads to greater weight loss than drugs like metformin after only 16 weeks. These findings suggest that partaking in 5:2 IF could help to prevent T2D or keep it under control.
Diet Outperforms Pharmaceutical Drugs
To compare the effect of 5:2 IF and common anti-diabetes drugs, Chinese Academy of Medical Sciences researchers recruited individuals between the ages of 18 and 65. These individuals were newly diagnosed with T2D (within 1 year) and were not taking any anti-diabetes medicine. The participants were also overweight and had high hemoglobin A1c (HbA1c), a measure of average blood sugar levels, with high HbA1c indicating high blood sugar levels.
The participants were divided into three groups:
- 5:2 IF: For two nonconsecutive days of the week, women consumed 500 calories/day and men consumed 600 calories/day.
- Metformin group: This group was given 1 g/day of metformin, which was escalated to 2 g/day if well tolerated.
- Empagliflozin group: This group was given 10 mg of empagliflozin, another anti-diabetes drug.
The participants partook in their respective interventions for 16 weeks. As a result, all participants saw a reduction in HbA1c. While the empagliflozin group attained a 1.5% reduction and the metformin group attained a 1.6% reduction, the 5:2 IF group achieved a 1.9% reduction, which was significantly higher. These findings suggest that 5:2 IF can improve T2D and outperform metformin and empagliflozin.
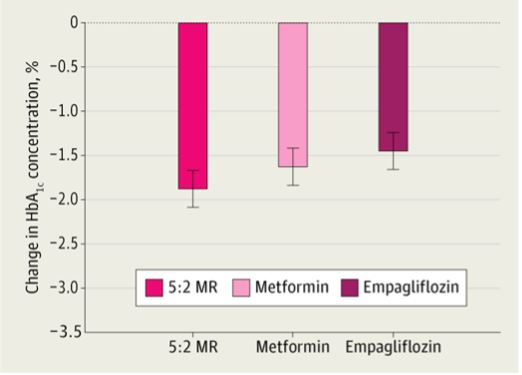
Usually, sugar, specifically glucose, is transported into our cells and utilized to make cellular energy. For this to happen, insulin must bind to iFurthermore, 80% of participants in the 5:2 IF group achieved HbA1C less than 6.5%, which is the clinical cut-off for T2D remission. In contrast, 60% and 55% of the participants achieved remission in the metformin and empagliflozin groups, respectively. Additionally, individuals in the 5:2 IF group lost significantly more weight, about 21 pounds on average, than individuals in the metformin and empagliflozin group, who lost about 12 pounds on average.
Overall, these findings suggest that 5:2 IF is just as good, if not better than metformin and empagliflozin in treating T2D, at least in newly diagnosed patients. Previous studies have shown that 5:2 IF can lower HbCA in individuals with T2D more than diets involving continuous energy restriction (1,200-1,500 calories every day). Furthermore, 5:2 IF lowered HbCA1 in T2D patients being treated with insulin. These studies suggest that 5:2 IF can help manage T2D. More studies will be needed to determine if 5:2 IF outperforms metformin and empagliflozin in long-term T2D patients.
How Does HbC1A Measure Blood Sugar Levels?
Usually, sugar, specifically glucose, is transported into our cells and utilized to make cellular energy. For this to happen, insulin must bind to insulin receptors on the outside of our cells. The binding of insulin activates a signal that leads to the movement of glucose transporters to the outer membrane of our cells. Once glucose transporters are within the outer membrane, glucose is permitted to enter our cells from the bloodstream.
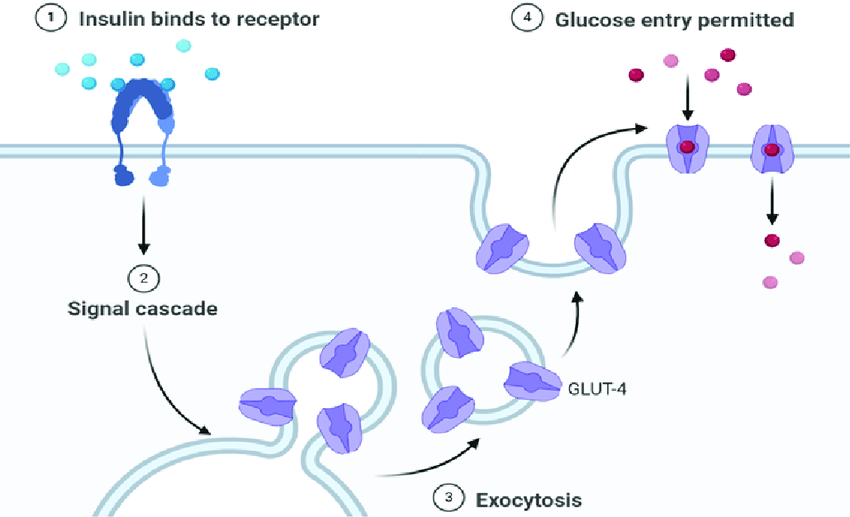
However, a lack of physical activity and excess body fat, especially around the waist, changes our cells’ metabolism. This metabolic alteration prevents our cells from placing glucose transporters into the outer membrane in response to insulin—insulin resistance. As a result of insulin resistance, glucose builds up in the bloodstream, eventually leading to T2D, characterized by high blood glucose levels. The concentration of glucose in our blood directly relates to HbAC1 levels.
Sugars, like glucose, can “stick” to proteins and other molecules through a process called glycation. In turn, the glucose in our bloodstream can attach to hemoglobin, the oxygen-carrying proteins in our red blood cells. This glycated hemoglobin is called HbAC1 and higher blood glucose concentrations lead to higher levels of HbAC1. It follows that HbAC1 levels can be thought of as the percentage of hemoglobin coated in sugar.
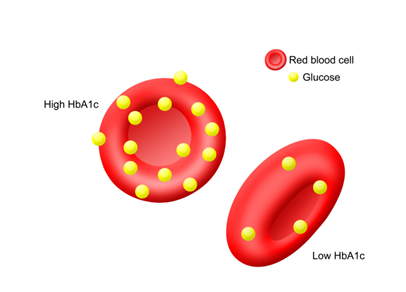
(Image: rch.org) HbA1c. HbA1c levels represent the amount of glycosylated hemoglobin proteins or the amount of sugars attached to red blood cells.
Preventing Diabetes to Live Longer
A major risk factor for T2D is being overweight and this risk increases with age. Therefore, maintaining a healthy weight by not consuming excess calories and adopting an active lifestyle is the best way to prevent or reverse T2D. Furthermore, T2D is associated with a 1.3- to 2-times greater risk of death, mostly from heart disease. Thus, preventing T2D increases the chances of living a longer life.

