German Scientists Call for A New Era of Life- and Health- Extending Medicine
Highlights
- The German National Academy of Sciences proposes shifting the German healthcare system towards preventing aging itself.
- Such a paradigm shift could influence the policy of other countries that face the same problem: a rapidly growing aging population.
- The proposal highlights known longevity-promoting compounds, including senolytics and the mTOR inhibitor rapamycin.
As we age, how do we ensure not just longer lives, but healthier ones? The German National Academy of Sciences Leopoldina, the oldest continuously existing academy of natural sciences and medicine in the world (founded in 1652), addresses this critical question in its recent discussion paper. This bold document proposes a paradigm shift in healthcare, moving away from merely treating diseases as they arise, towards actively preventing them by targeting the very process of aging itself.
The Looming Challenge of an Aging World
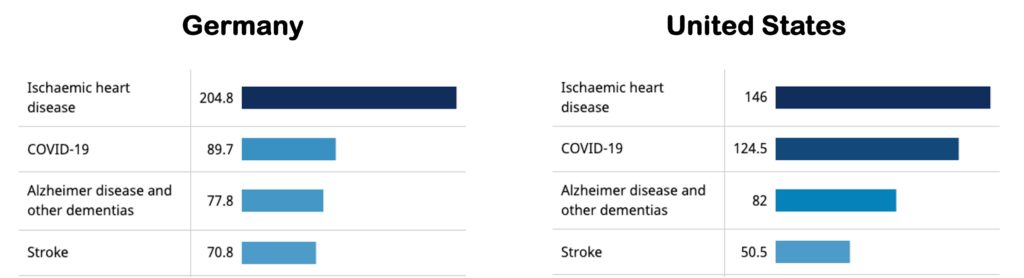
Germany faces the same problem as the rest of the industrialized world, including the United States: A future where a significant portion of the adult population is over 65. If things continue as they are, such a demographic shift will leave a large proportion of the population suffering from multiple chronic, age-related diseases (e.g., cardiovascular disease, dementia, and cancer).
This multimorbidity places immense strain on healthcare systems, economies, and individual well-being, exacerbating inequalities and poverty. The traditional approach of managing individual diseases, while necessary, is becoming increasingly unsustainable in the face of this growing challenge.
But what if we could tackle the root cause? What if we could intervene at the biological level of aging to prevent these diseases from taking hold in the first place? This is the ambitious vision put forth in the Leopoldina paper. It argues that decades of research into the biology of aging have revealed profound insights, demonstrating that it is indeed possible to extend “healthspan” – the period of life spent in good health.
Shifting the Paradigm: From Treatment to Prevention
The core of the Leopoldina’s proposal lies in a fundamental reorientation of medical practice. Instead of a reactive approach, where medicine responds to illness, they advocate for a proactive, preventative strategy. This involves understanding and manipulating the biological mechanisms that drive aging to prevent the onset of age-related diseases. This is the essence of “geroprotective medicine” – a field dedicated to treating the aging process itself, rather than its myriad of manifestations. To achieve this transformative goal, the paper outlines four key proposals:
Bolstering Basic Research
The foundation of this new medical frontier lies in a deeper, more comprehensive understanding of the biology of aging. This means investing significantly in fundamental research to unravel the intricate mechanisms that govern how our bodies age. The more we understand these processes, the more effectively we can design interventions to promote healthy aging.
Accelerating Translation
Scientific discoveries, no matter how profound, only make an impact when they are translated into practical applications. The paper emphasizes the importance of translating biological knowledge from the laboratory bench to the clinic, developing geroprotective pharmaceutical interventions that can prevent diseases before they begin.

Geroscience-Driven Clinical Trials and Biobanks
To ensure that these new interventions are safe and effective, rigorous clinical trials are essential. These trials must be specifically designed to assess the impact of treatments on the aging process. Furthermore, the establishment of accessible national biobanks, housing vast multi-omics datasets (information from genes, proteins, metabolites, etc.), will be crucial. These resources will provide the evidence base needed to develop and validate health maintenance and disease prevention strategies.
Integrating Geromedicine
The ultimate aim is to integrate geromedicine into mainstream medical practice. This means that preventing disease by treating aging becomes a central tenet of healthcare, offering a powerful tool to address the health crisis that is inevitable with a rapidly expanding elderly population.
Senotherapeutics
The good news is that research has already provided promising avenues for intervention. The paper points to “senotherapeutics” – compounds that eliminate the harmful effects of senescent cells. Progress in geroscience has revealed that the accumulation of senescent cells in our body promotes chronic inflammation and organ damage. Thus, senescent cells are considered one of the root causes of aging. Studies have shown that eliminating senescent cells with senolytics mitigates age-related diseases. Senomorphics, which inhibit the production of the harmful molecules secreted by senescent cells, have also shown similar effects.
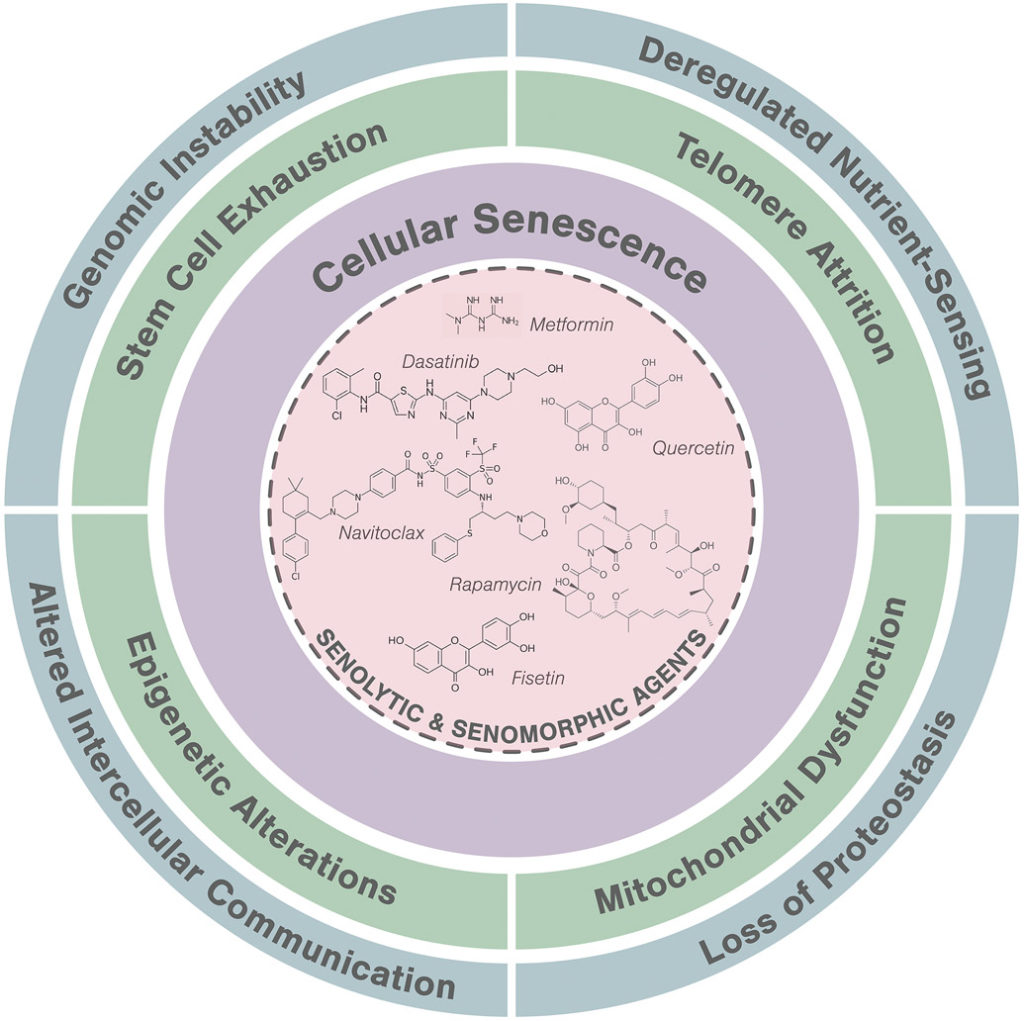
To tackle known fundamental age-related problems like senescent cells with senotherapuetics (senolytics and senomorphics), the proposal calls for establishing collaborative research networks. The NIH-funded SenNet Consortium in the United States serves as an excellent model, integrating researchers and leveraging existing strengths to create comprehensive atlases of senescent cells. Such networks facilitate data sharing and open science, accelerating discovery by making data accessible to the broader research community.
Reevaluating Existing Drugs
Moving forward, the Leopoldina paper emphasizes several critical elements, including a systems approach and a holistic view. Aging is a complex, whole-organism phenomenon. Therefore, research needs to adopt systems approaches, integrating data from various biological levels to understand how specific mechanisms affect complex signaling networks. This also means considering factors like sex, early life conditioning, psychosocial stress, nutrition, and environmental exposures, all of which influence aging trajectories.
Interestingly, some existing metabolic drugs, such as GLP-1R agonists (e.g., semaglutide) and SGLT2 inhibitors (e.g., glifozines) appear to work at the systems level. They have shown unexpected “geroprotective” effects – reducing the risk of multiple chronic age-associated diseases. The paper suggests that further investigation into how these drugs impact the underlying mechanisms of aging could lead to new insights and improved interventions. Since these drugs have already been approved by the FDA, they are essentially repurposed geroprotective drugs.
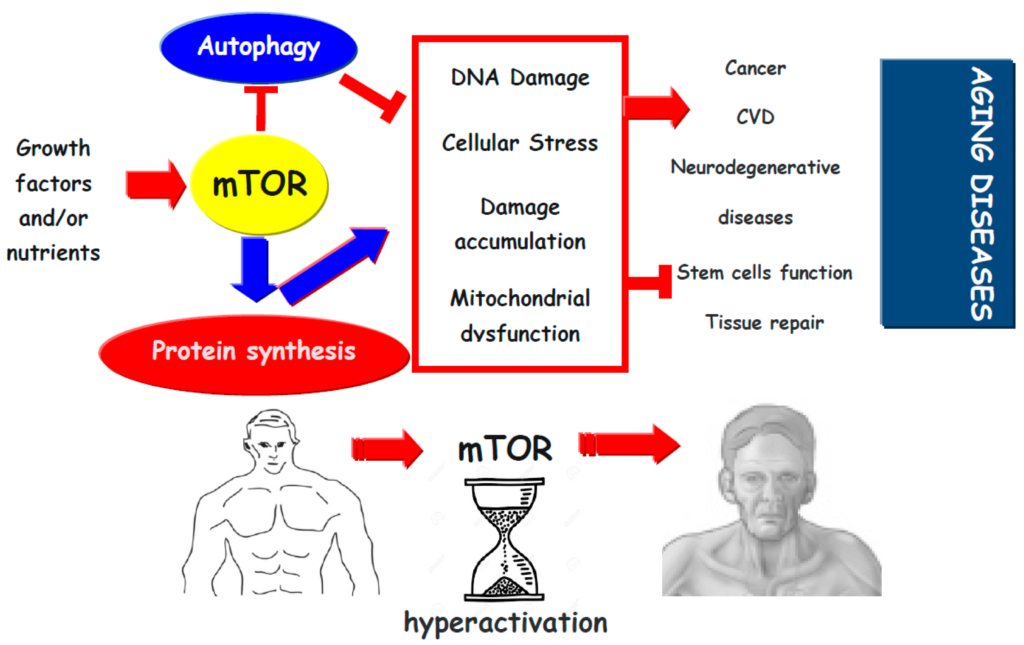
Similar to GLP-1R agonists and SGLT2 inhibitors, an mTOR inhibitor called rapamycin has also been repurposed and tested as a geroprotective drug. Inhibiting mTOR, a nutrient sensor and regulator of growth, has been shown to extend the lifespan of multiple model organisms while counteracting age-related diseases. This may be why rapamycin is one of the compounds highlighted by the Leopoldina.
A Healthier Future for All Ages
The Leopoldina discussion paper paints a compelling picture of a future where medicine is not just about extending life, but about extending healthy, vibrant life. By focusing on the biology of aging and by fostering robust research, collaborative networks, and innovative therapeutic approaches, we can move closer to a society where age is no longer synonymous with chronic illness. This shift towards health-extending medicine holds the promise of a healthier, more inclusive future for generations to come.

