Harvard Scientists Propose Using Fecal Transplants from Our Younger Selves to Reverse Aging
Harvard researchers introduce the concept of banking fecal matter during our healthy years to rejuvenate our gut microbes later in life and treat age-related disease.
Highlights
- Changes in the way we live and eat over the last few decades have changed the composition of our gut microbes – the microbiome.
- Microbiome changes have been associated with a higher incidence of conditions like digestive ailments, type 2 diabetes, and cardiovascular disease.
- To restore a healthier microbiome and mitigate diseases, researchers propose storing fecal matter from a younger age for intestinal transplantation later in life.
The industrialization and urbanization of human societies over the past few decades have changed the way we live and eat, leading to drastic alterations in our microbiomes. Numerous conditions ranging from asthma and digestive tract issues to type 2 diabetes and heart complications have been associated with these alterations. This has led scientists to the idea of “rewilding” the human microbiome – restoring it to an ancestral state – by reconstructing ancient microbial compositions from the guts of mummies or hunter-gatherers from nonindustrial societies and transplanting them to present-day humans. What if we could find a simpler and more well-defined way to achieve the same goal of rejuvenating the microbiome by populating it with microbes from a younger, more healthy gut?
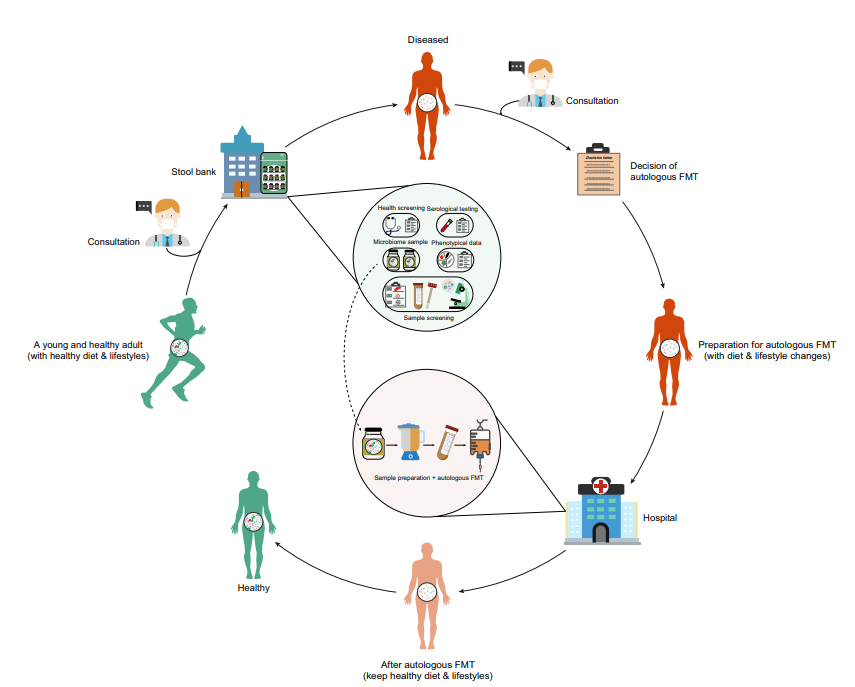
Published in an opinion article in Trends in Molecular Medicine, Liu and colleagues from Harvard Medical School propose that banked feces from a younger age could be used to rejuvenate the microbiome later in life through transplantation (autologous fecal microbiota transplantation [autologous FMT]). The Harvard-based team proposes that autologous FMT is a safer alternative to current procedures – transplanting fecal matter from healthy donors to aged individuals (heterologous fecal microbiota transplantation [heterologous FMT]). Liu and colleagues also cover with somewhat limited detail the procedures by which people can bank their fecal matter at a young age for later use. The Harvard researchers claim that, if following a proper diet and exercise regimen, autologous FMT may offer a new way to overcome diseases associated with an altered microbiome.
Why the New Fecal Transplant Method could be Better than the Old
Heterologous FMT has gained popularity in the past few decades for its ability to treat conditions like inflammatory bowel disease (IBD) and a gut bacterial infection called Clostridioides difficile infection (CDI). However, there have been long-term safety concerns for recipients, challenges with donor recruitment and screening, and struggles with FDA regulation.
A major safety concern arising from heterologous FMT is the possibility that donors and recipients are not compatible. Genetic and dietary mismatches can lead to variabilities in response to treatment and potentially adverse immune responses, especially in immunocompromised recipients. Naturally, this concern is avoided with autologous FMT because the donor and recipient are one and the same.
Some studies have already examined the effect of autologous FMT on treating disease, showing that it is less effective than heterologous FMT in treating digestive disorders. However, in these studies, stool samples were collected from patients at the time of their treatment or shortly before their sickness rather than before disease onset. Liu and colleagues propose that collecting fecal matter at a young, disease-free age of 18-35 years would be ideal and would likely confer much better results.
Stool Banking Procedure
While using autologous FMT from a young age to prevent disease later in life is now just a hypothesis without experimental evidence, it is something that can be implemented now. To bank fecal matter for transplantation later in life, individuals should first consult a physician. Once a health screening that evaluates dietary intake, medications, and lifestyle is complete, a stool sample of about 55 grams will be collected for each future gut microbiome rejuvenation. When the stool samples have been collected, they will be frozen through a cryopreservation procedure. To protect proteins and DNA within the fecal matter from degradation, the stool sample is typically stored with liquid nitrogen at -1960C.
Challenges to Stool Banking Complicate Its Feasibility
Some fundamental challenges remain for rejuvenating the human gut microbiome, which will need to be addressed with extensive animal and human studies. For example, we do not yet know whether a transplanted microbiome will retain its youthful characteristics for long periods of time. Another question that we need to address is how many of us will be eligible for and hence truly benefit from rejuvenating our microbiomes.
The cost of banking our fecal matter is another practical issue that needs to be worked out since no sources currently provide a dollar amount for autologous FMT. A fecal matter banking center called OpenBiome does offer heterologous FMT from a healthy donor for around $2,050 per fecal capsule dosage.
“We do not anticipate that all individuals in our society are willing or able to pay the cost associated with the service of ‘rejuvenating’ their gut microbiome,” said Liu in a press release. “But as scientists our job is to provide a scientific solution that may eventually benefit human well-being. Developing a reasonable business model and pricing strategy so that the solution is affordable to everyone would require the joint force of entrepreneurs, scientists, and perhaps governments.”

