Female Mouse Infertility Remedied by NMN
Age-associated mitochondrial DNA point mutations reduce oocyte quality in humans, providing a potential biomarker for embryo viability in assisted reproduction
As mammals age, fertility decreases and our ability to procreate drops. This fall in fecundity is thought to be linked with the accumulation of mutations in mitochondria, the powerhouses of the cell. These ancient cell structures have their own genetic code that is passed almost exclusively from mother to offspring through the oocyte—the immature egg cell in the ovary that is the very beginning of human life. But if and how aging accumulated mitochondrial DNA mutations in oocytes modulate fertility remains unknown.
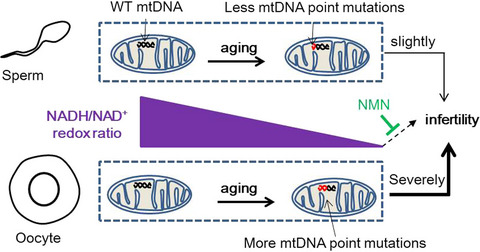
Yang and colleagues from the Chinese Academy of Sciences published an article in Aging Cell comparing the quality of oocytes in young (under 31 years old) and elder (over 37 years old) female patients. Their research showed that aged women had more mitochondrial DNA point mutations in oocytes and a lower rate of forming blastocyst—the developmental stage at which embryos are transplanted into the womb. Importantly, these mitochondrial DNA mutations were linked to a decrease in female mice’s fertility by reducing ovarian primordial and mature follicles—small ovarian sacs that secrete hormones.
How this happens is that the accumulation of mitochondrial DNA mutations decreases fertility by impairing the oocyte’s balance in the levels of a vital molecule central to cellular energy generation called nicotinamide adenine dinucleotide (NAD+) and a highly related form called NADH. Importantly, this imbalance could be rectified by adding nicotinamide mononucleotide (NMN) to drinking water to rescue oocyte quality. This research points to NMN as a candidate therapeutic option for oocyte aging to promote fertility in older women or those with metabolic disorders.
Why does fertility decline with age?
Aging is one of the key factors in both male fertility and female fertility. Indeed, female fertility normally peaks at age 24 and diminishes after 30, with pregnancy occurring rarely after 50. Mitochondrial malfunction has been proposed to play important roles in age- and environment-induced infertility. For instance, mitochondrial DNA deletions have been reported to accumulate in human ovarian aging.
As a result, the assessment of mitochondrial function status and mitochondrial DNA content and integrity is often performed to investigate the quality of oocytes in assisted reproductive technologies. But the links among aging, mitochondrial DNA mutations, and infertility remain not fully understood.
Human fertilization drops with age-related gains in mitochondrial mutations
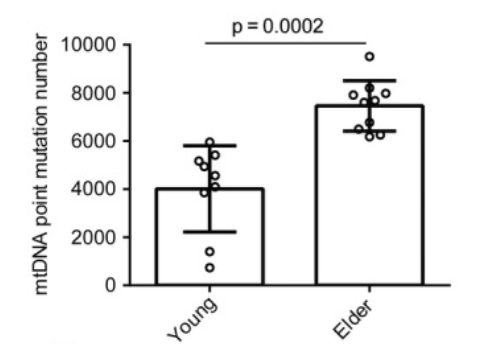
For the first time, Yang and colleagues quantified the effect of aging on the accumulation of mitochondrial mutations in human individual oocytes using next-generation sequencing (NGS).
They examined immature oocytes discarded during intracytoplasmic sperm injection (ICSI) from women younger than 31 years old and older than 37 years old for different mutation types in mitochondrial DNA.
Point mutations—a mutation affecting only one or very few nucleotides in a gene sequence—were detected as the most abundant mutations in older female patients. This study also showed that mitochondrial DNA point mutations inversely correlate with oocyte quality, providing a potential biomarker for embryo viability in assisted reproduction.
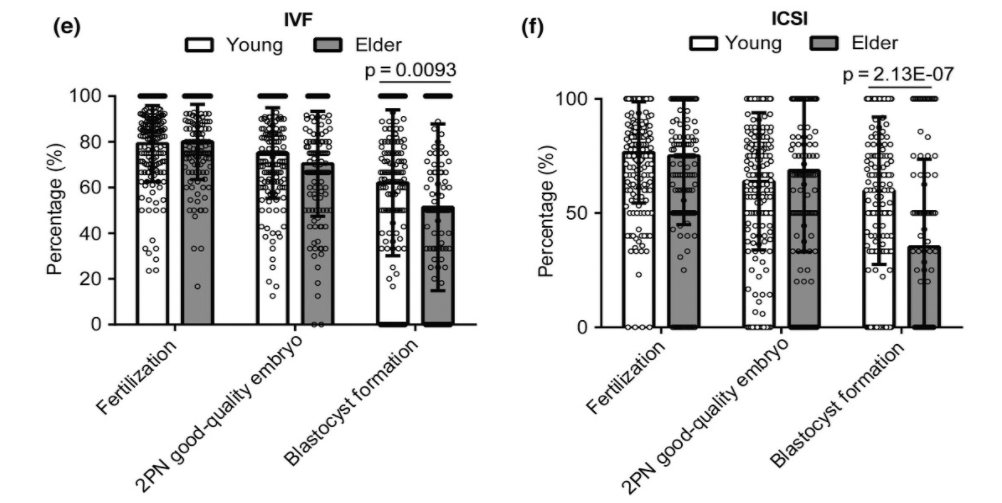
Next, the researchers examined which step of fertilization is affected by age in patients undergoing in vitro fertilization (IVF) or ICSI. Although the fertilization rates showed no significant differences between young and elder participants, the formation rate of blastocysts in the elder group was significantly lower than that of the young group in both IVF and ICSI cycles.
This study answers the fundamental question—which step of oogenesis is damaged by age-related mitochondrial DNA mutations—and suggested follicles could be the potential therapeutic target for female infertility. “Collectively, our results indicate that elder female patients have defects in blastocyst formation correlated with an increased accumulation of oocyte mitochondrial DNA point mutations,” said the authors.
Mitochondrial mutations alter the NADH to NAD+ ratio
Next, the researchers wanted to know what was tying the mitochondrial mutation rate to oocyte quality. They used a genetically altered mouse that accumulates 7 to 10 times the level of mitochondrial DNA deletions and a 2500-fold higher level of point mutations compared to unaltered mice. This mouse model allows a detailed examination of the causal role of mitochondrial DNA mutations in age-related fertility and its dependence on sex.
They demonstrated that mitochondrial DNA mutations decrease female mice’s fertility by impairing the oocyte’s ratio of NADH to NAD+. Notably, the oocytes from elder mice showed a similarly perturbed ratio of NADH to NAD+.
NMN recovers fertility in mice with mitochondrial mutations
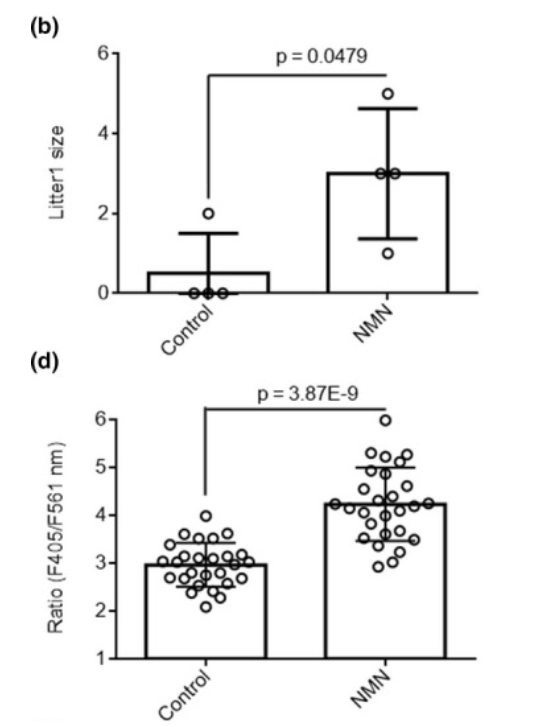
Treatment with NMN, a key NAD+ intermediate, elevated the amount of NADH in oocytes of genetically modified mice that accumulate mitochondrial DNA mutations. The unchanged amount of NAD+ with the up-regulation of NADH indicated that the ratio of NADH to NAD+ in oocytes of these genetically modified mice was increased by NMN treatment.
Yang and colleagues then wanted to test if the recovery of NADH to NAD+ levels by NMN in oocytes had effects on mouse fertility. To do so, they examined the litter sizes of the genetically modified mice that gain mitochondrial DNA mutations that were given drinking water supplemented with NMN. What they saw was that the mice that were drinking water with NMN (900 mg/kg/day) had larger litter sizes than those that did not. This result indicates that NMN is remarkably capable of ameliorating infertility in these female mice.
Can NMN be used to aid reproduction in humans?
These findings show that NMN has potential as a therapeutic option for mitochondrial DNA mutations in oocytes. “Our study, by systematically comparing the quality and mitochondrial DNA mutations of oocytes in young and elder female patients, showed that mitochondrial DNA point mutations inversely correlate with oocyte quality, which provides another potential biomarker for embryo viability in assisted reproduction, and demonstrated NMN as a potential candidate drug for oocyte aging caused by mitochondrial DNA mutation,” said the researchers.
It is important to note that the mouse model used here was not an aging model per se but, in fact, a mitochondrial mutation model. These findings will need to be replicated in a more robust model of aging prior to being applied to human subjects and in assisted reproduction.