NMN Improves Cell Survival and Reduces Inflammation in Dry Eye Disease
Treatment of cells modeling dry eye disease with NMN improves their viability by dampening inflammatory marker activation.
Highlights
- NMN treatment protects eye cell viability under conditions of dry eye disease moisture loss.
- NMN preserves eye cells by activating DNA maintenance and metabolic health-promoting protein Sirtuin1 (SIRT1).
- NMN triggers immune cells called macrophages to transition from states of cell killing to healing.
Dry eye disease is one of the most prevalent eye disorders and causes substantial discomfort to those who have it. Inflammation and excessive salt concentrations in tears – a damaging condition called hyperosmolarity that causes cells to lose moisture – lead to eye surface injuries and possible visual impairment. Dry eye treatment strategies include eye drops with artificial tears that target discomfort, but researchers still need to find ways to preserve eye cell function following hyperosmolarity damage. Research has shown that the molecule nicotinamide mononucleotide (NMN) provides cell protection in eye disorders like retinal detachment, so finding out whether this can apply to dry eye disorder is crucial.
Zhu and colleagues from Changshu Number 2 People’s Hospital in China published a study in the Journal of Inflammation Research describing how treating eye cells from mice exposed to salt-induced hyperosmolarity with NMN preserves their viability. NMN reduces the level of eye cell inflammation after hyperosmolarity exposure by activating a protein important in metabolism and DNA integrity preservation called Sirtuin1 (SIRT1). According to their study, NMN also orchestrates eye immune cells to transition from a state of cell killing and elimination to a state of healing. If these findings translate to humans, NMN could provide a means to prevent eye injury from dry eye disease.
How Does NMN Protect Against Dry Eye Disease?
NMN increases levels of the vital molecule nicotinamide adenine dinucleotide (NAD+), which is involved in cell energy-generating reactions and is used by SIRT1 for its functions in promoting healthy metabolism and maintaining DNA integrity. Researchers believe that by increasing NAD+, NMN protects eye cells from injury in conditions like retinal detachment. For these reasons, finding out the effects of NMN in dry eye disease conditions and the pathways it influences remain paramount.
NMN Enhances Eye Cell Survival Under Dry Eye Conditions
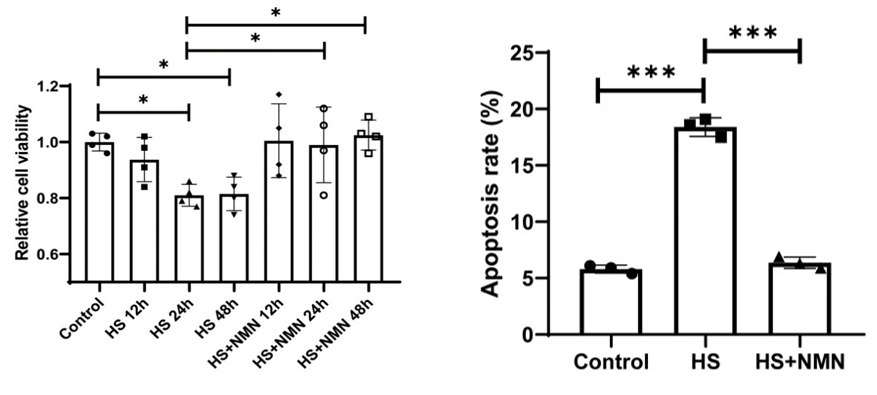
To see whether NMN protects mouse eye cells from a salt-induced hyperosmotic laboratory dish environment, Zhu and colleagues treated them with 500 µM of NMN and measured their survival. The research team found NMN treatment prevented cell death from hyperosmotic stress. These findings indicate that NMN has a significant protective effect on eye cells under hyperosmotic stress in conditions similar to dry eye disease.
NMN Activates SIRT1 to Protect Eye Cells
Zhu and colleagues then sought to understand how NMN reduces inflammation. They found NMN diminishes levels of the inflammation-associated substance IL-17a in hyperosmotic stress conditions. The research team also found that SIRT1 levels increase with NMN treatment in the hyperosmotic conditions and that applying a SIRT1 inhibitor further aggravated inflammation marker levels. These findings suggest that NMN reduces inflammation in hyperosmotic conditions by increasing and activating SIRT1.
NMN Facilitates an Immune Cell Healing Response
To further explore how NMN protects eye cells, Zhu and colleagues examined the effects of NMN and an inhibitor of the inflammatory marker IL-17a on the state of immune cells called macrophages. These immune cells can exist in two states. When macrophages are in an M1 state, they tend to kill cells in their proximity, and when in an M2 state, they heal cells close to them. The researchers found a hyperosmotic environment increased the destructive M1 macrophages, while NMN and the IL-17a inhibitor promoted the healing M2 macrophages under the same conditions. These experiments show that NMN suppresses macrophage killing and promotes healing by inhibiting a prominent marker for and driver of inflammation, IL-17a.
“These findings provide us important clues in the understanding of the effects of NMN on [dry eye disease] development,” stated Zhu and colleagues in their publication. “We provided the knowledge of NMN application on the expression of SIRT1 and Il-17a and then described the potential molecular mechanism.”
Can NMN Help Human Dry Eye Disease?
Future studies examining NMN in human cells will tell whether people can use this therapeutic agent to protect themselves from hyperosmolarity in dry eye disease. If so, NMN treatment in combination with artificial tear eye drops may slow the progression of injuries from this common eye ailment.

