NMN vs NR: Scientists Rejuvenate COVID-19 Infected Cells
NMN and NR similarly rejuvenate human blood vessel cells by preventing oxidative stress — a driver of aging — and restoring nitric oxide, critical for blood vessel function.
Highlights:
- In human artery cells infected with SARS-CoV2, NAD+ and nitric oxide (NO) levels are low, and reactive oxygen species (ROS) are high, indicating oxidative stress.
- NR prevents NO production loss and elevations in ROS.
- NMN prevents elevations in ROS and nearly prevents NO production losses.
Coronavirus 2019 (COVID-19) is now one of the world’s leading causes of death. Interestingly, COVID-19 survivors have an increased risk of cardiovascular disease (CVD), which is strongly related to the severity of infection. However, researchers from the University of Colorado Boulder may have found a way to counter these CVD risks by replenishing NAD+.
As reported in Nitric Oxide, Freeberg and colleagues show that NMN and NR enhance NO production and prevent oxidative stress in blood vessel cells exposed to plasma from hospitalized patients with COVID-19. The authors conclude:
“NAD+ precursors may represent a promising approach to prevent [blood vessel cell (endothelial)] dysfunction and reduce the risk of CVD after COVID-19.”
NMN and NR Rejuvenate COVID-19 Blood Vessel Cells
To study blood vessels, Freeberg and colleagues examined human cells from the aorta — the largest artery in the body. For their studies, the researchers chose endothelial cells, which make up the innermost layer of the aorta. These human aorta endothelial cells (HAECs) generate nitric oxide (NO), a gaseous signaling molecule that dilates blood vessels.
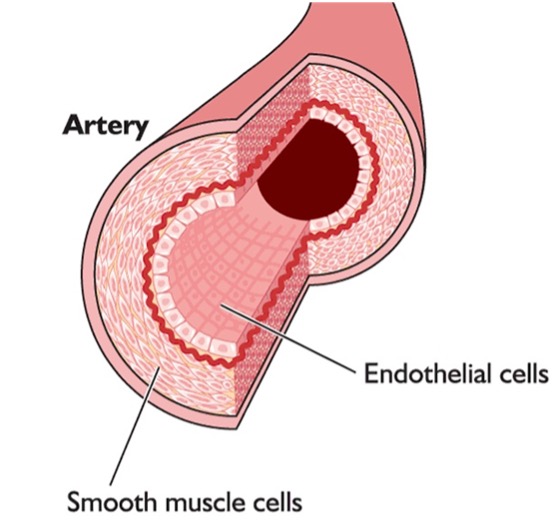
(Image: Lonza Biosciences) Blood Vessel (Artery) Layers. The innermost layer of our aorta is made of endothelial cells, which produce nitric oxide (NO), a gas that easily moves across cell membranes. NO signals middle-layer smooth muscle cells to relax, dilating the aorta to allow for increased blood flow.
To determine the effect of COVID-19 on human blood vessel cells, the researchers infected HAECs with the SARS-CoV-2 virus. As a result of infection, the COVID-19 HAECs produced more reactive oxygen species (ROS), which when excessively elevated cause damage to cells — a phenomenon known as oxidative stress. The COVID-19 HAECs also produced less NO and had low NAD+ levels. These findings reveal that low NAD+ levels are associated with COVID-19 blood vessel dysfunction.
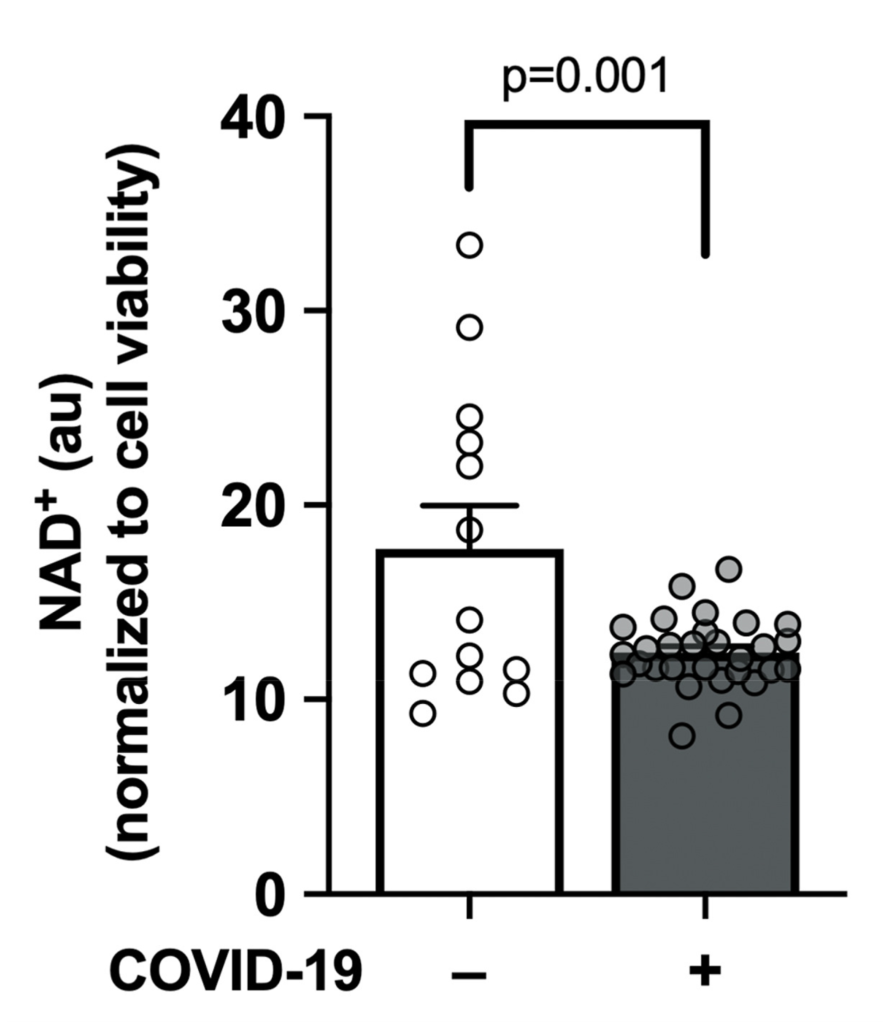
(Freeberg et al., 2023 | Nitric Oxide) COVID-19 Lowers Blood Vessel Cell NAD+. Compared to normal blood vessel cells (white), infected COVID-19 blood vessel cells (gray) have lower NAD+ levels.
To see if replenishing NAD+ could rejuvenate the COVID-19 HAECs, Freeberg and colleagues treated the cells with the NAD+ precursor nicotinamide riboside (NR). It was found that NR brought NO and ROS levels back to normal. These findings suggest that NR rejuvenates COVID-19 HAECs.
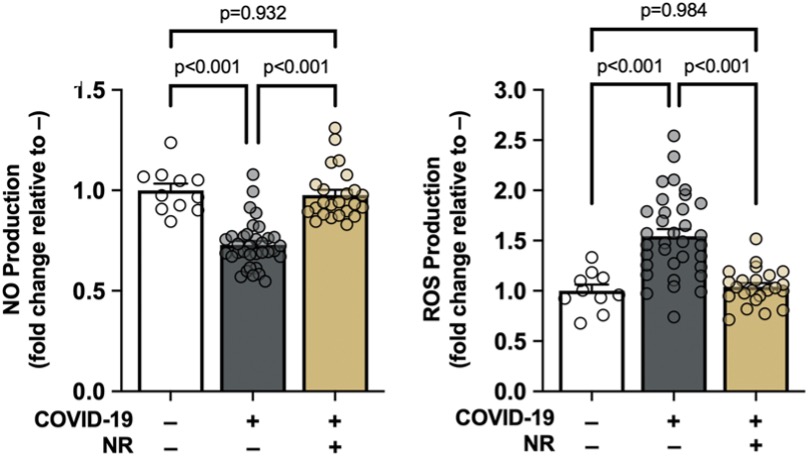
(Freeberg et al., 2023 | Nitric Oxide) NR Rejuvenates COVID-19 Blood Vessel Cells. Compared to infected COVID-19 blood vessel cells (gray), infected COVID-19 blood vessel cells treated with NR (gold) exhibit normal (white) levels of NO and ROS production.
In addition to NR, Freeberg, and colleagues treated another group of COVID-19 HAECs with nicotinamide mononucleotide (NMN). NMN was shown to increase NO production almost to normal levels. NMN also reduced ROS production to statistically normal levels. These findings suggest that NMN rejuvenates COVID-19 HAECs like NR.
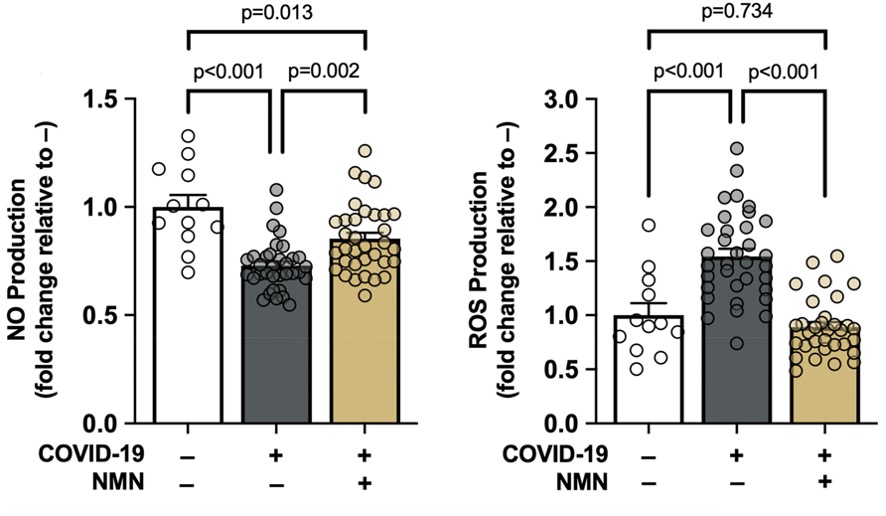
(Freeberg et al., 2023 | Nitric Oxide) NMN Rejuvenates COVID-19 Blood Vessel Cells. Compared to infected COVID-19 blood vessel cells (gray), infected COVID-19 blood vessel cells treated with NR (gold) exhibit normal (white) levels of ROS production and near-normal levels of NO production.
Overall, the findings of Freeberg and colleagues suggest that replenishing NAD+ prevents oxidative stress and NO depletion in COVID-19 HAECs, which could prevent cardiovascular dysfunction and disease.
A recent study showed similar results with NMN lowering ROS levels in human endothelial cells. Additionally, the study showed that NMN reduced senescence — a pro-inflammatory state that may drive aging.
NMN vs NR: The Saga Continues
While NMN did not increase NO to statistically normal levels, it came very close. This statistical difference could be due to the number of cells tested for each NAD+ precursor. Thirty-two COVID-19 HAECs were treated with NMN and twenty-three were treated with NR. This means the results for the NMN group, having more cells, are more statistically accurate. Furthermore, adding more cells to the NR group could increase variability to the point where its average for NO production is similar to NMN.
There are very few studies that have tested the effect of NMN against NR, especially in humans. One study that mixed NMN or NR with other ingredients found the two similarly improved the metabolism of healthy adults. In the case of the walking longevity experiment, Bryan Johnson saw similar effects from NMN and NR. Therefore, until more studies comparing NMN and NR are conducted, it seems like neither NMN nor NR is better than the other.

