Phase I Trial Results Show Safety of Nicotinamide-Expanded Donor-Derived Natural Killer Cells in Blood Cancers
Gamida cell announces study data of nicotinamide-expanded donor-derived natural killer cells in patients with refractory non-Hodgkin lymphoma and multiple myeloma.
Cell-based therapies take cells and inject, graft, or implant them into a patient for a medicinal effect. They are recognized for their tremendous potential to provide curative treatment options for patients with blood cancers and rare, serious blood disorders. One potential candidate for cell-based therapies is an immune cell type called natural killer cells that swiftly eliminate nearby cells. Therapies with natural killer cells offer tremendous potential for transforming the care of blood cancers. However, to create effective treatments with natural killer cells, they must be expanded in the laboratory while maintaining therapeutic potency and functionality.
Gamida Cell Advances Natural Killer Cell Therapies
Gamida Cell Ltd., a leading cellular and immune therapeutics company, announced updated data from the ongoing Phase I clinical study (NCT03019666) of GDA-201, an investigational, cell-based cancer therapy that uses natural killer cells. In this Phase I clinical trial, Gamida Cell reported safety data in patients with relapsed or refractory non-Hodgkin lymphoma and multiple myeloma, cancers that originate from white blood cells called lymphocytes and plasma cells, respectively. Gamida Cell said that Phase II studies to test for safety and efficacy in a larger cohort of patients with aggressive and indolent non-Hodgkin lymphoma are planned.
Gamida Cell has pioneered a new approach with the goal to improve treatment outcomes beyond what is possible with cell-based therapies derived from donors. Their proprietary platform can expand multiple cell types, including natural killer cells, while maintaining their original function and potency. This approach enables Gamida Cell to administer a therapeutic dose of natural killer cells to patients.
Gamida Cell’s proprietary platform increases the number and lifespan of donor-derived natural killer cells that can fight cancer by exposing them to a small molecule called nicotinamide, a form of vitamin B3 or niacin. According to the company’s website, natural killer cells grown with nicotinamide multiply faster, live longer, and are particularly good at producing inflammatory molecules and recruiting other immune cells into tumors than normal natural killer cells.
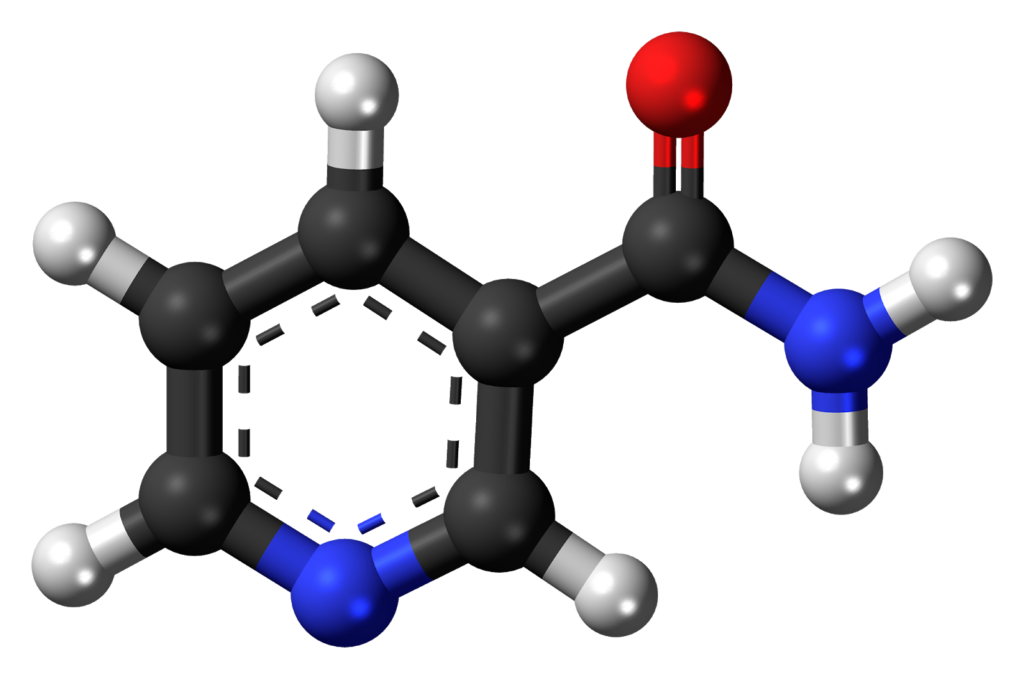
Nicotinamide (NAM) is a form of vitamin B3 found in food and used as a dietary supplement and medication.
Gamida Cell applied the capabilities of its nicotinamide-based cell expansion technology to develop GDA-201, a natural killer cell-based therapy for the treatment of blood and solid tumors in combination with standard of care antibody therapies. GDA-201 is a novel natural killer cell product derived from natural killer cells from healthy donors that have been expanded in culture with nicotinamide and a molecule that stimulates natural killer cells called IL-15.
GDA-201 addresses key limitations of natural killer cells by increasing their ability to eliminate cancerous cells and to be retained and replicated in a recipient’s bone marrow and lymphoid organs. Gamida Cell previously reported that GDA-201 improved the killing function, proliferation, and resistance against exhaustion of natural killer cells in animal models before clinical trials in humans.
This Phase I clinical study was commissioned primarily to evaluate the safety of GDA-201 in a small group of human patients with relapsed or refractory non-Hodgkin lymphoma and multiple myeloma. Participants aged 18 to 70 with non-Hodgkin’s lymphoma or multiple myeloma who have failed prior treatments were able to enroll at the Masonic Cancer Center in Minnesota. In total, 30 patients were enrolled: 15 with non-Hodgkin lymphoma and 15 with multiple myeloma, in 3 cohorts of escalating GDA-201 dose. Fifteen of the patients received the maximum target dose.
The investigators did not observe dose-limiting toxicities. The most common adverse events were abnormally low levels of platelets (thrombocytopenia), high blood pressure (hypertension), abnormally low number a type of white blood cell called neutrophils (neutropenia), and insufficient healthy red blood cells (anemia). There was no damage to the brain or peripheral nervous system (neurotoxicity). Also, there were no adverse immune effects, such as the large, rapid release of cytokines into the blood from immune cells (cytokine release syndrome), the attacking of stem cells in the bone marrow (marrow aplasia), or graft versus host disease. One patient died of E-coli sepsis, a life-threatening condition caused by the body’s unbalanced response to an infection that triggers changes causing multiple organ systems.
They also reported efficacy outcomes in patients with non-Hodgkin lymphoma. In patients with non-Hodgkin lymphoma, the overall response rate was 73.3% and the median duration of response was 8.7 months (range 4.3-25 months). One-year estimates of progression-free survival and overall survival were 66% and 82%, respectively.
These results show that cellular therapy using GDA-201 with monoclonal antibodies to enhance antibody-dependent cellular toxicity was well-tolerated, and demonstrated significant clinical activity in heavily pretreated patients with advanced non-Hodgkin lymphoma. These data support the future testing of multiple infusions of GDA-201 to potentially enhance the anti-tumor effect.

