Predicting Age-Related Diseases with the Apple Watch: New Study Confirms Reliability
Scientists have revealed that smartwatch technology is capable of predicting the risk of aging and age-related diseases—and it could help you live longer.
Highlights
- Using artificial intelligence to analyze data from Apple Watch users, researchers predicted each user’s age with an error of less than 3 years.
- Predicted biological age was used to determine the probability of age-related diseases, such as diabetes and heart disease.
- The watch was also used to show how biological age changes in response to smoking, exercise, and sleep.
For decades, researchers have searched for reliable ways to measure biological aging. While chronological age counts the number of years we’ve lived, biological age reflects the actual condition of our body. Two 50-year-olds can have drastically different biological ages—one with the physiology of a 40-year-old, another of a 60-year-old.
Crucially, biological age predicts health outcomes far better than chronological age. It can reveal who’s at higher risk for disease, who might benefit from interventions, and whether lifestyle changes or treatments are actually working to slow aging. The challenge? Most aging biomarkers require expensive blood tests, invasive procedures, or clinical equipment. DNA methylation clocks—the gold standard in aging research—require lab analysis of genetic material. Brain MRI scans cost thousands of dollars. These methods are impractical for regular monitoring throughout daily life.
The Power of Prediction
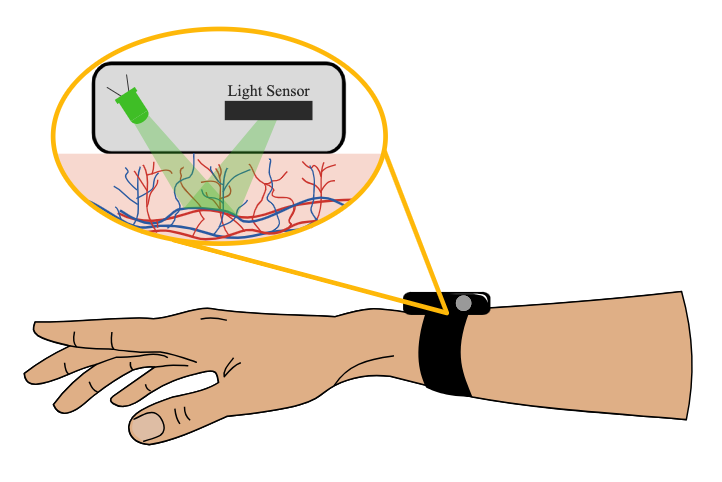
Enter photoplethysmography (Ppg)—a fancy term for shining green light onto the wrist and measuring how much is reflected back. As blood pulses through the vessels of the wrist with each heartbeat, the amount of reflected light changes. Smartwatches use this technology to calculate heart rate, but the full waveform contains more information. In a recent publication, researchers analyzed Ppg data from 213,593 individuals from the Apple Heart & Movement Study. They found that smartwatch Ppg can be used to determine the biological age of participants.
As we age, our cardiovascular system changes in predictable ways. Arteries stiffen. The heart’s pumping efficiency declines. Blood vessel walls thicken. These changes alter the shape of the Ppg waveform in subtle but measurable ways. Using advanced deep learning, the researchers trained an AI (artificial intelligence) model to detect these age-related patterns. In doing so, they were able to predict the chronological age of healthy individuals with a mean error of just 2.4 years—comparable to or better than expensive clinical tests. This Ppg and AI-determined age has been dubbed PpgAge.
Looking Older Than Your Years: A Warning Sign
PpgAge is essentially one’s biological age, which, in healthy individuals, should be the same as chronological age. However, not everyone is healthy, i.e., free of diseases. Thus, the difference between PpgAge (predicted biological age) and chronological age (actual age)—called the “PpgAge gap”—reveals crucial health information.
The Apple and Princeton University researchers found dramatic associations between elevated PpgAge gaps and disease. Among 35–45-year-old men, those whose biological age appeared more than 6 years older than their actual age had a heart disease diagnosis rate 3.5 times higher than average. For diabetes in women of the same age group, appearing 6+ years older was associated with a 2.4-fold increased diagnosis rate.
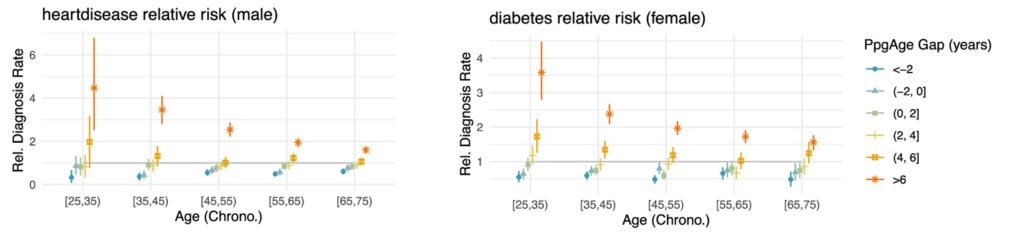
Even more compelling, PpgAge gap predicted future health problems. When researchers followed participants over time, controlling for traditional risk factors like blood pressure, cholesterol, and smoking, an elevated PpgAge gap significantly predicted who would develop heart disease, hypertension, diabetes, and high cholesterol. In some cases, the predictive power of PpgAge gap matched or exceeded conventional risk factors.
The Lifestyle Connection: Your Daily Choices Show Up in Your Biology
Perhaps the most actionable findings relate to lifestyle factors. PpgAge revealed clear patterns connecting daily behaviors to biological aging. Daily smokers appeared significantly older than never-smokers, with the gap widening with age. By ages 55-65, daily smokers’ biological age was about 3.5 years older than that of never-smokers of the same chronological age. Former smokers fell somewhere in between, suggesting that quitting may allow some recovery.
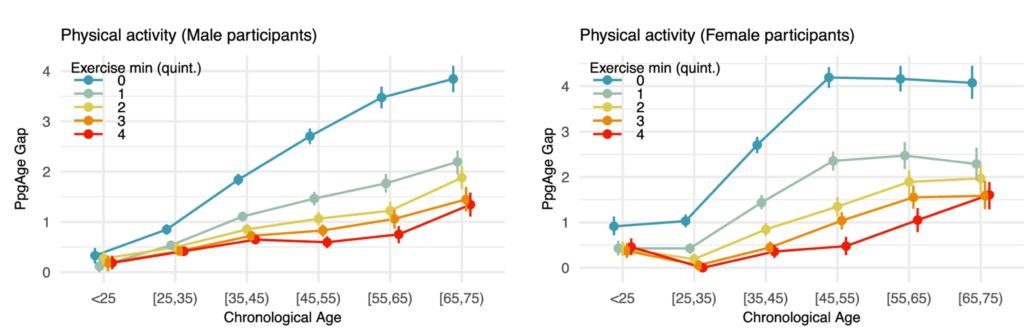
Physical activity showed a powerful protective effect. Participants in the lowest quintile of exercise (the least active 20%) appeared substantially older than their more active peers, with differences growing larger in older age groups. Among 65–75-year-old men, the least active appeared nearly 4 years older biologically, while the most active appeared only 1.3 years older than their chronological age.
Quality matters as much as quantity. Participants with longer deep sleep duration, shorter time to REM sleep, and higher sleep efficiency all showed younger biological ages. Each additional hour of deep sleep was associated with being nearly a year biologically younger. These findings suggest that PpgAge is capturing the accumulated impact of how life is lived.
Real-Time Aging: Watching Biology Change
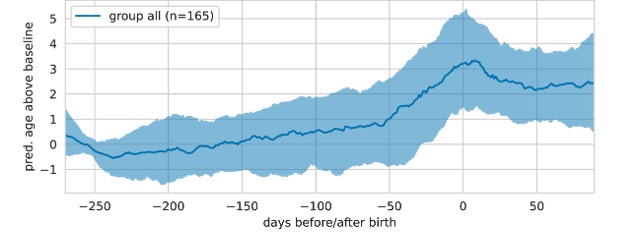
One of the most remarkable aspects of wearable-based aging clocks is the ability to track changes over time. The researchers documented how PpgAge increases during major physiological events. During pregnancy, women’s biological age increased by a median of 3.6 years, with sharp increases in the final trimester. This aligns with recent findings from DNA methylation studies showing pregnancy temporarily accelerates biological aging—though questions remain about long-term recovery.
Following heart attacks, bypass surgery, or valve replacement, many participants showed increases in PpgAge of 1.7 to 2.5 years over six months, suggesting these events may accelerate aging processes. This longitudinal sensitivity is a game-changer. Unlike a once-yearly blood test, a wearable aging clock provides continuous monitoring. You could potentially see the impact of starting an exercise program, improving sleep habits, or undergoing treatment in near real-time.
The Future of Personalized Longevity
The development of PpgAge may contribute to changing how we approach healthy aging:
- Accessible Monitoring: Millions already own compatible devices. No clinic visits, no blood draws, no expensive tests—just passive data collection during daily life.
- Early Intervention: Detecting accelerated aging before disease develops creates opportunities for prevention. If your biological age is trending upward, you could work with your doctor to identify and address risk factors early.
- Testing Interventions: PpgAge could be used to assess whether experimental interventions actually slow aging. Does that new supplement work? Does time-restricted eating help? Instead of waiting decades for mortality data, changes in biological age could provide answers in months.
- Personalized Insights: Population averages only tell part of the story. Continuous monitoring reveals your individual aging trajectory and which interventions work for your unique biology.
Important Caveats and Future Directions
While exciting, PpgAge has limitations worth noting. The study participants were Apple Watch users in the United States—a relatively affluent, tech-savvy population that may not represent everyone. Medical history relied on self-reporting, which can be inaccurate. The longest follow-up was four years, relatively short in aging research terms.
The researchers also note that PpgAge appears to capture primarily cardiovascular aging. While cardiovascular health strongly influences overall longevity, aging is multidimensional. Brain aging, immune system aging, and metabolic aging may require complementary approaches. Additionally, the relationship between PpgAge and behavioral factors is observational. People who exercise more might differ in unmeasured ways from sedentary individuals. Randomized controlled trials would strengthen causal claims about which interventions truly modify biological age.

