Scientists Reveal Vitamin D Prevents Knee Arthritis Via Anti-aging Proteins
Knee osteoarthritis in old mice deficient in vitamin D was prevented by vitamin D supplementation due to its effects on the activity of Sirt1 – an anti-aging, longevity protein.
Highlights:
- Mice with vitamin D deficiency develop osteoarthritis faster than their age-matched counterparts, but supplementing these mice with vitamin D alleviates the osteoarthritis.
- Chondrocytes – cells thatmake cartilage – which have been exposed to inflammatory molecules and treated with vitamin D show decreased cell aging and cellular stress, both implicated in the development of osteoarthritis.
- The decreased cell aging and stress are likely due to the increased Sirt1 seen in cells treated with vitamin D.
Vitamin D has long been under investigation for its use in the treatment of osteoarthritis – the degenerative breakdown of cartilage and changes in the underlying bone. However, a consensus regarding the utility and mechanism of action of vitamin D in osteoarthritis has never been reached. A recent study shows that vitamin D may have its effects on bones through sirtuin proteins, which are becoming known for their anti-aging properties.
The study, out of medical universities in China and published in the International Journal of Biological Sciences, focused on old and middle-aged mice who are vitamin D deficient. Chen and colleagues found that vitamin D deficiency led to accelerated development of knee osteoarthritis. Supplementing the mice with vitamin D3 rescued the osteoarthritis development. Furthermore, the researchers found that decreased Sirt1 – one of the sirtuin proteins – was also corrected with vitamin D3 supplementation. Sirt1 deficiency has been linked to increased spontaneous osteoarthritis, while increases in Sirt1 have been shown to increase the number of bone-forming cells, as well as promote the production of extracellular matrix (tissue that holds all the cells and proteins in proper formation). Sirt1 is also known to inhibit cell aging (senescence) and inhibit the production of cells thatpromote senescence and inflammation, which can further exacerbate and promote osteoarthritis.
“This study therefore not only identifies novel mechanisms of [vitamin D] deficiency in accelerating age-related knee [osteoarthritis] development, but may also provide experimental and theoretical evidence for potential utilization of [vitamin D3] or downstream targets, including Sirt1 activators to prevent age-related knee [osteoarthritis],” the investigators wrote.
Vitamin D3 Supplementation Prevents Osteoarthritis
Chen and colleagues took 6-month-old and 12-month-old mice – about 34 and 58 in human years, respectively – some of which were vitamin D deficient, and fed them a high calcium and phosphate diet, which are both necessary for bone formation. This diet, known as the rescue diet, helped normalize calcium and phosphate levels in the mice but did not affect vitamin D levels. The mice who were vitamin D deficient – due to the loss of protein necessary to change the inactive form of vitamin D into its active form – had more cartilage destruction and erosion, as well as extracellular matrix loss, than age-matched controls. Additionally, the vitamin D-deficient mice had more osteoarthritis based on the OARSI osteoarthritis scale – a standard assessment used to determine the severity of osteoarthritis.
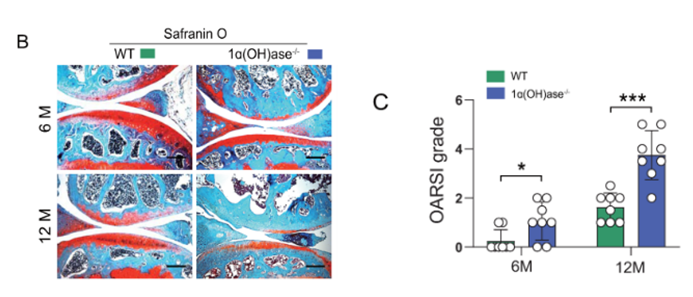
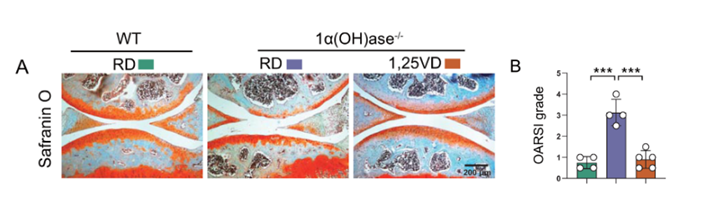
The researchers sought to determine whether supplementing the vitamin D-deficient mice with vitamin D would prevent osteoarthritis. The deficient mice were fed either the rescue diet or the rescue diet with vitamin D3 injections from about three weeks of age until 12 months. The deficient mice treated with vitamin D3 had less cartilage destruction, cartilage erosion, and extracellular matrix loss than the untreated deficient mice. OARSI scores were also rescued by vitamin D supplementation. Furthermore, levels of inflammatory signaling molecules and proteins involved in cartilage breakdown were reduced with vitamin D supplementation.
Vitamin D3 Benefits are due to Sirt1 and the Vitamin D Receptor
Using human chondrocytes – the cells that produce cartilage –, the scientists found that vitamin D supplementation increased the amount of vitamin D receptors (the protein that helps vitamin D interact with cells) under inflammatory conditions. IL-1β, which was used to induce the proinflammatory conditions, has been shown to induce osteoarthritis due to increased oxidative stress – cellular stress caused by reactive oxygen molecules – and cellular senescence. Furthermore, vitamin D supplementation served to prevent the inflammation-induced reduction in chondrocyte viability, as well as reactive oxygen molecules and cellular senescence.
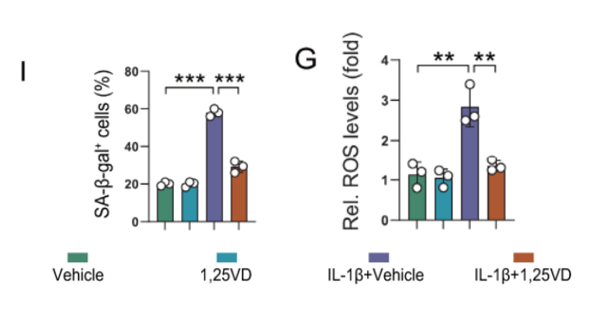
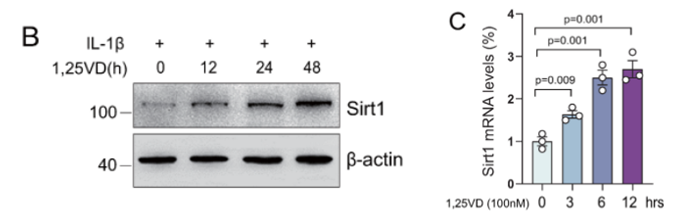
The investigators found that vitamin D3 treatment, even in the presence of IL-1β, increased the amount of Sirt1 protein in a time-dependent manner. Further analysis showed that the vitamin D receptor could interact with the genes promoting Sirt1 protein production, further suggesting a strong link between vitamin D and Sirt1. Vitamin D3 supplementation also inhibited the accumulation of reactive oxygen molecules in the chondrocytes while increasing the number of chondrocytes and decreasing cellular senescence. Additionally, increasingSirt1 activity in mesenchymal stem cells – cells responsible for repairing and replenishing the bone cells – also helped prevent osteoarthritis development in vitamin D deficient mice, further cementing the downstream role of Sirt1 in vitamin D deficiency-induced osteoarthritis.
Vitamin D and Health
Chen and colleagues show here how vitamin D reduces osteoarthritis through Sirt1, suggesting a role for vitamin D in preventing age-related cartilage changes.
Other studies have shown the value of vitamin D in promoting healthy aging. Vitamin D deficiency has been shown to increase aging via its effects on epigenetics – the way in which your environment can change how your genes are read and made into proteins. Additionally, vitamin D supplementation – in combination with exercise and omega-3s – has been shown to reduce cancer risk. However, it is also known that vitamin D tends to decrease with age, leading to the need for more studies into the benefits of supplemental vitamin D.
This study shows how vitamin D supplementation can benefit bone health, but more long-term studies are needed before we can fully understand the ways in which vitamin D supplementation can assist in maintaining our health as we age. There are minimal side effects of taking moderate amounts of vitamin D; however vitamins can interact with other medications, so please speak with a healthcare provider before stopping or starting any medications or supplements.
Model: wild-type and 1α(OH)ase-/- male mice
Dosage: vitamin D – 1 microgram per kilogram of body weight

