Scientists Unveil Results from Human Trial Directly Comparing Three NAD+ Precursors
A direct comparison of NAD+ precursors in humans shows that NMN and NR double circulating NAD+ after two weeks of supplementation, while Nam does not.
Highlights
- NMN (nicotinamide mononucleotide) and NR (nicotinamide riboside) approximately double circulating NAD+ levels after 14 days of supplementation, while Nam (nicotinamide) only does so acutely at four hours after supplementation.
- The study provides evidence that gut bacteria convert NMN and NR to NA (nicotinic acid), a potent NAD+ booster, to increase circulating NAD+ levels.
- The data also show that NMN and NR modulate gut bacteria to increase the concentrations of short-chain fatty acids (SCFAs), which are believed to strengthen the gut barrier and reduce systemic inflammation.
As published in Nature Metabolism, Cuenoud and colleagues from Nestlé Health Science in Switzerland present evidence that the NAD+ precursors NMN and NR double circulating NAD+ levels after 14 days of supplementation, while nicotinamide does not. Moreover, their data support that, rather than directly increasing NAD+ levels, gut bacteria convert NMN and NR to NA, a potent NAD+ booster, to raise circulating NAD+. Furthermore, the researchers’ data suggest that NMN and NR modulate gut bacteria to increase concentrations of short-chain fatty acids (SCFAs), metabolites of gut bacteria that have been shown to have anti-inflammatory, anti-diabetes, and anticancer effects in rodents. These findings suggest that NMN and NR sustainably raise circulating NAD+ to a comparable degree and that, through their modulation of gut bacteria, NMN and NR increase SCFA concentrations to promote gut health and other physiological benefits.
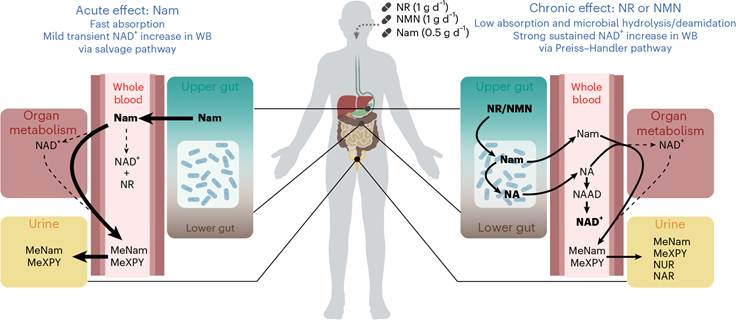
“This head-to-head comparison of three NAD+ precursors in healthy adults shows that NR and NMN are comparable in their ability to chronically increase baseline whole-blood NAD+ levels, while Nam provides only an acute transient effect,” say Cuenoud and colleagues in their publication. “Our findings suggest that, contrary to Nam, NR and NMN are not directly absorbed in the systemic circulation but are slowly metabolized by the microbiota to NA, a very potent NAD+ precursor in whole blood.”
No head-to-head comparisons of different NAD+ precursors’ effects on NAD+ levels had been done before this human trial from Cuenoud and colleagues. As such, they chose three prominent NAD+ boosters, Nam, NR, and NMN, for comparison and left out NA since it is associated with skin flushing and gastrointestinal issues at high doses.
Aside from comparing the three NAD+ precursors’ effects on NAD+ levels, the researchers sought to test whether the NAD+-boosting effects of NR and NMN come from their conversion to NA by gut microbes. This was because studies with rodents have suggested that gut microbes convert NR and NMN to NA, which potently raises circulating NAD+.
NR and NMN Double NAD+ After 14 Days, But Nam Does Not
To directly compare the effects of administering the three NAD+ precursors, the Swiss research team analyzed 65 adults with an average age of 34.7 years. The researchers administered NR to 16 of these participants, NMN to 15, Nam to 17, and a placebo to 17. The doses administered were 1 gram of NR, 1 gram of NMN, 0.5 grams of Nam, or the placebo daily for 14 days.
Interestingly, after 14 days of supplementation, NR and NMN significantly increased circulating NAD+ by about two-fold, while Nam had no significant effect. These findings suggest that NR and NMN have similar effects in sustainably raising circulating NAD+ levels.

To get an idea of how the NAD+ precursors affect NAD+ levels over shorter time periods, Cuenoud and colleagues analyzed NAD+ levels in whole blood over four hours after administration. They found strikingly different effects; Nam most significantly increased blood NAD+ levels. This finding suggests that while NR and NMN increase blood NAD+ over the course of 14 days, Nam has a more significant effect in acutely increasing NAD+ levels.
Cuenoud and colleagues also assessed blood metabolites following supplementation with the three NAD+ precursors. They found that NR and NMN raised levels of metabolites associated with gut microbes. This finding suggested to the researchers that NR’s and NMN’s effects on gut microbes may play a role in their effects in raising blood NAD+ levels.
To evaluate the possible conversion of the NAD+ precursors to metabolites of gut microbes, Cuenoud and colleagues analyzed fecal-derived gut microbes from healthy adults in laboratory dishes. For their experiment, the researchers exposed the gut microbes to NR for 48 hours.
The research team found that the microbes rapidly converted NR to Nam and then further converted Nam to NA, resulting in a significant, sustained concentration of NA over the course of 24 hours. This effect was consistent with previous experiments in rodents, which demonstrated that after oral intake, NR is converted to Nam and then NA by gut microbes.
Cuenoud and colleagues further analysed whether NR or Nam treatment modulates gut microbe metabolite production and composition. They found that NR, but not Nam, significantly increased SCFAs, metabolites demonstrated to have anti-inflammatory, anti-diabetes, and anti-cancer properties in rodents. This effect was accompanied by a higher total gut bacterial density after exposure of gut microbes to NR for 48 hours. Also, NR increased the amount of a specific gut bacterial species called Enterocloster aldensis. These findings suggest that taking NR increases SCFA concentrations to possibly confer systemic aging intervention effects and that the gut bacterial species Enterocloster aldensis metabolizes NR in the gut to raise circulating NAD+.
Finally, the Swiss researchers ran a similar test with gut microbes from healthy adults to find whether gut bacteria metabolize NMN similarly to NR. They found that, indeed, NMN’s conversion to Nam and then NA was similar to NR’s. They also showed that NMN modulated gut microbes similar to NR. These results suggest that, alongside NR, NMN is converted to Nam and then NA to increase circulating NAD+ and that it increases SCFAs, which may mitigate gut inflammation and promote gut health.
Collectively, the data from Cuenoud and colleagues led the team to propose a human model where NR and NMN are metabolized in the gut by microbes, giving rise to NA, which boosts NAD+ levels in the blood. In contrast, Nam is directly absorbed and metabolized, transiently increasing NAD+ levels. Whether this means that NR and NMN work more effectively than Nam to confer effects against aging awaits longer testing with human trials. However, a key indicator that Nam may not work as well as NR or NMN may come from the evidence that Nam did not increase SCFAs from gut microbes like NR and NMN did.
As such, NR and NMN’s capabilities to increase SCFAs from gut bacterial metabolism could be a key way that these two NAD+ precursors may work against aging in humans. Only future studies examining the long-term effects of NR and NMN supplementation can discern whether this is the case.
The Case for Liposomal NR or NMN
The results suggest that gut bacteria metabolize NR and NMN and convert them to NA to raise circulating NAD+, which helps build the case for taking liposomal forms of these NAD+ precursors, which are widely available for purchase. Liposomes are tiny fat bubbles that encapsulate NR or NMN and protect these molecules from digestive degradation, allowing for significantly higher absorption. Through their capabilities to protect NR and NMN from digestive degradation, liposomes may ensure that these NAD+ precursors make it to the gut, where gut bacteria may convert them to NA and potently and sustainably raise circulating NAD+ levels.
Moreover, some researchers have labeled declining NAD+ levels with age as a hallmark of aging, associated with impaired function of the cell’s powerhouses (mitochondria), DNA damage, and metabolic disease. As the evidence presented in this study suggests, supplementing with NR or NMN may work better than Nam to counteract an age-related decline in NAD+.
At the same time, figuring out whether tissues and organs effectively absorb increased NAD+ levels from the bloodstream to counteract declining NAD+ levels throughout multiple organ systems will require further human testing. If NAD+ precursors do raise NAD+ levels in tissues and organs throughout the body, this could potentially have widespread effects, boosting mitochondrial function, enhancing DNA repair, and improving metabolism.
Some research reports that supplementing with NR increases NAD+ abundance in organs such as the brain and skeletal muscle; however, increased NAD+ levels in various tissues have not been consistently observed in all studies. Hence, future human trials could directly compare the effects of supplementation with NR, NMN, and NAM on NAD+ levels in multiple organ systems to confirm whether these NAD+ precursors indeed increase NAD+ levels throughout the body.
Model: 65 healthy adults (32 males and 33 females with an average age of 34.7 years)
Dosage: 1 g of NR, 1 g of NMN, or 0.5 g of Nam taken orally daily for 14 days

