A Nutrition Guide for Memory Loss Care and Prevention
When equipped with the right dietary guidelines, vitamins, and social support from close relatives, senior adults can help mitigate and prevent loss of memory. This comprehensive guide shares some of the most simple tactics when it comes to battling disorders that target a person's memory.
Preface
Memory
problems are a major issue facing senior adults in the United States. In fact,
as many as 40% of U.S. adults over the age of 65 experience memory
impairments as they age. On top of being inconvenient or frustrating, memory loss
can have a variety of health consequences, ranging from minor issues to
potentially life-threatening problems — including malnutrition.
Malnutrition is one of the most common and serious risks associated with memory
impairments in senior adults. In addition to natural processes, like the slowing of your
metabolism and decreased nutrient
absorption, memory impairments of any kind can make it difficult for them to get
the nutrients they need to thrive.
Maintaining adequate nutrition is crucial to ensuring a high quality of life as
people get older. Whether your loved one hasn’t yet experienced memory loss or
they’ve been diagnosed with a memory loss disorder, it’s crucial to know more
about how to use their diet to prevent further memory problems and support
overall brain health.
Memory Loss and Eating Habits
Memory
loss is a broad term that encompasses many different situations, health
conditions, or impairments related to your brain’s ability to remember details
or events. It can be short-term or long-term, temporary or permanent. Memory
problems have a variety of causes, such as head injuries, alcohol consumption,
or other physical and mental health conditions.
For many senior adults, memory loss is a natural and normal part of the aging
process. For others, memory loss can take the form of a diagnosable disorder,
such as Alzheimer’s disease or dementia.
No matter the cause, memory impairments can have a profound impact on
eating habits. Common changes and impacts include:
- Forgetting to eat or drink;
- Forgetting how to eat or drink;
- Forgetting how to cook;
- Forgetting how to use utensils and cookware;
- Loss of appetite due to medications or a change in dosage;
- A diminished sense of smell or taste;
- Not recognizing or enjoying food;
- Having difficulties or pain while chewing and swallowing;
- Being unable to communicate what you want to eat, or that you are hungry.
This is not a comprehensive list of the ways memory impairments can affect eating habits. Just as memory loss can vary, so can its impacts on your loved one’s eating habits, desire to eat, or ability to eat. Be mindful of how your patient feels about food, and pay attention to any difficulties they may face with eating.
Overcoming Common Eating Difficulties
There are several ways you can offer support and assistance to a loved one or patient who is struggling with eating. Different eating problems have unique symptoms and causes, and therefore require equally unique solutions. It’s important to focus on addressing the specific difficulties your loved one faces and finding something that works well for their needs.
Loss of Appetite
Loss of appetite is a common result of memory problems and memory disorders. Some reasons you may experience loss of appetite include not recognizing the feeling of hunger, experiencing a mental health issue (such as depression) that suppresses appetite, taking a medication that reduces appetite, or simply forgetting to eat.
Consider trying the following strategies to encourage eating and stimulate appetite:
- Eat meals at the same time each day so they’re part of a routine;
- Eat smaller meals and snacks more frequently throughout the day;
- Serve exciting, enticing foods that have different colors or pleasant aromas;
- Serve favorite and familiar foods;
- Serve different kinds of foods or varieties of cuisine;
- Serve food at the appropriate temperature, such as making sure soup is warm or a salad is cool;
- Prepare foods with herbs, spices, and sauces to add more flavor;
- Make mealtime fun and enjoyable, such as creating a pleasant atmosphere or making it a social event.
If the above methods don’t work for your loved one, you can always talk to a doctor about medications that can help stimulate an appetite.
Difficulty Chewing or Swallowing
Memory loss can also lead to difficulties with chewing or swallowing food. This issue is more common in people who have late-stage Alzheimer’s or dementia, but pain or troubles with chewing and swallowing can impact anyone with memory loss.
Here are some best practices to follow for issues with chewing and swallowing:
- Avoid foods that are difficult to chew and swallow, such as popcorn, nuts, carrots, apples, and bread with hard crusts;
- Incorporate more soft foods that are easy to chew and swallow, like yogurt, oatmeal, smoothies, very ripe fruit, scrambled eggs, or soup;
- Cut foods up into smaller pieces so they’re easier to chew;
- Have your loved one sit up straight, with their head leaning forward, to make it easier to swallow and reduce choking hazards;
- Check their mouth when they’re done eating to make sure all food has been swallowed.
Make sure you or someone in your home is familiar with the Heimlich maneuver, in case choking blocks your loved one’s airways. Even if you do know the Heimlich maneuver, always call 9-1-1 for help if your loved one is choking.
Tactile and Grasping Difficulties
Many senior adults experience issues with coordination and motor skills, especially if they have memory loss. They may have trouble grasping utensils and cups, or forget how to use them properly.
Tactile and grasping problems can be more difficult to overcome, but some helpful ideas include:
- Show them how to use utensils by modeling the behavior, such as showing them how to eat soup with a spoon;
- Cut food up into small pieces so they can eat it with their fingers or a spoon;
- Serve foods that don’t require utensils, such as sliced fruit and vegetables, sandwiches, chicken nuggets, or hamburgers;
- Use utensils and plates that your loved one feels more comfortable with or can use more easily.
If they have continued or escalating difficulties, you can work with an occupational therapist to help improve their motor skills. You can also look for adaptive utensils, cups, and plates that are designed to make eating and drinking easier for individuals with tactile, gripping, or motor difficulties.
Vision Impairment
Memory
loss does not directly cause vision problems in and of itself. Just as it’s
common to experience age-related memory loss, senior adults may also experience
age-related vision loss.
However,
Alzheimer’s has been
linked to several eye diseases, including glaucoma, age-related macular
degeneration, and diabetic retinopathy. While researchers do not fully
understand the relationship between these diseases, individuals with these
three eye diseases are more likely to develop dementia or Alzheimer’s.
Whatever the cause, vision impairment can make eating difficult, especially if
the vision loss is relatively new or sudden. To assist someone with impaired
vision at mealtimes, try the following:
- Use high-contrast place settings, such as a dark tablecloth and a white plate, to make them easier to see;
- Place the plates, utensils, and cups in the same spot at each meal;
- Explain where food is located on a plate compared to the face of a clock (for example,
- Explain where the beverage, butter, salt and pepper, or other items are in relation to the plate.
There may also be adaptive tools and equipment available that can help people with low vision eat more easily. Be patient while you both adjust to this new normal.
Behavior Changes and Irritability
Memory loss can result in behavioral changes, emotional shifts, and irritability. Researchers estimate that anywhere from 30% to 90% of people with dementia experience behavioral disturbances, including agitation, aggression, and disinhibition.
You may notice behavioral changes or increased irritability in your loved one at mealtimes. They may refuse to eat, insult the food, spit food out, or otherwise act out. Dealing with these shifts can be difficult and unpleasant, but there’s often a reason motivating this behavior, such as:
- They dislike the food or drink;
- They think the food or drink is too hot or too cold;
- The environment or eating area is overwhelming or unpleasant;
- They feel pressured or rushed to finish their meal quickly or in a certain amount of time;
- They don’t want help, or feel they don’t need help, eating or drinking;
- They feel frustrated by their difficulties, either with eating or memory loss in general.
Remain
calm and level-headed during any instances of irritability or anger. Remember
that your loved one isn’t upset with you, and know that you are in a position
to help them resolve this issue. Keep an eye on their body language and facial
expressions to look for potential signs of irritation or frustration.
Don’t offer food or drink when they’re still upset. Instead, wait until they
calm down to do so. Do your best to create a calm and pleasant experience, so
they don’t feel stressed about finishing their meal.
Dehydration
Similar
to malnutrition, senior adults are at a
greater risk of dehydration. Frequently, senior adults become less aware of the
sensation of thirst. This can cause them to drink less water, even though they
still need the same amount to stay properly hydrated. Memory loss can increase
this risk, as senior adults may forget to drink liquids throughout the day or
forget how to drink.
Dehydration can have devastating health impacts; in extreme cases, it can be
deadly. Further, dehydration can reduce
cognitive functioning — including memory — potentially worsening the effects of
memory loss disorders. Simply put, staying properly hydrated is an absolute
necessity for all senior adults.
Here are a few ways to help senior adults stay hydrated and avoid the effects of dehydration:
- Start and end each day by drinking a glass of water;
- Start each meal with a glass of water;
- Take small sips of water between bites during meals;
- Eat foods with high water content, such as watermelon, tomatoes, cucumbers, spinach, and zucchini;
- Avoid dehydrating drinks, such as caffeinated and alcoholic beverages;
- Use an app or mobile device to track their water intake and provide hydration reminders;
- Drink something other than water, such as juice or milk, on occasion;
- Infuse water with fruit or a calorie-free flavoring to add variety;
- Bring a refillable water bottle when you leave the house so you can stay hydrated throughout the day;
- Order water from restaurants or when eating out.
In addition, you should pay attention to their water intake and try to look out for any signs of dehydration.
Considerations for Severe Dementia or Alzheimer’s
Eating
can be especially challenging if your loved one has severe memory loss. They
may feel confused or overwhelmed by food, or forget how to eat and drink
entirely. Forgetting how to eat and swallow is common in the late stages of
dementia and Alzheimer’s disease.
Consider trying the following techniques to help someone with severe memory
issues eat:
- Model how to eat by doing so yourself, such as demonstrating how to bring food to your mouth and chew;
- Guide them through the eating process, step by step;
- Assist them with the physical act of eating;
- Remove any decorations or items that resemble food from the living area to reduce confusion and distractions (such as plastic fruit or laundry soap packets).
For additional guidance specific to your loved one, be sure to talk with their doctor about how you can support their eating.
Additional Tips To Encourage Healthy Eating Habits For Seniors With Memory Loss
Whether your loved one has minor memory loss or has been diagnosed with a memory disorder, here are a few best practices that can help foster healthy eating habits:
- Get them involved with meal preparations. If they’re able, ask them to help you cook or set the table.
- Encourage them to exercise or be more physically active. There are countless ways senior adults can benefit from exercise, but it can be especially helpful for stimulating appetite and making food more enjoyable.
- Give them choice and independence when it comes to food. Ask them what they want to eat or drink, and let them decide when and where they want to eat.
- Make eating a social event with friends or family members, so it’s more fun and enjoyable.
- Make sure the eating area is free of any clutter and mess. Reduce distractions by turning off the TV or radio.
- Play calming music or music that your loved one enjoys.
- Use appropriate lighting. Bright lights might be irritating or distracting, but dim lighting could make it difficult for your loved one to see their food.
- Use whatever utensils, plates, bowls, or cups are easiest for your loved one to manage, even if it’s not the “right” way to use them (for instance, using a spoon to scoop up vegetables).
- Make meals as relaxed and leisurely as possible so they don’t feel rushed or stressed while eating.
- Don’t assume they’re full or finished eating if they stop mid-meal. They may be tired or have lost concentration and need a short break. They may also be embarrassed about their struggles with food.
- Serve meals at the time of day they are hungriest, or most alert and engaged, even if it is at an “unusual” mealtime.
- Make sure the food is at an appropriate temperature before serving. Further, serving food at the right temperature can make it more inviting to eat.
- Ask if they need help eating.
Again, everyone has different challenges when it comes to eating with a memory disorder. Not all solutions will work well for all people. Take your time to find a strategy that effectively supports your patient or loved one.
Senior Nutrition
Senior adults have different nutritional
needs
than younger individuals. Generally, they need to eat less, due to reduced
activity levels and slowed metabolism. However, the calories they do eat need
to be nutrient-rich in order to maintain adequate nutrition and overall
wellbeing. Because of the additional difficulties and challenges they face,
eating a nutritious diet is particularly important for senior adults who are
dealing with a memory disorder.
It’s best for senior adults to eat a variety of whole foods, including:
- Fruits and Vegetables: Serve a variety of fruits and vegetables each day. Try “eating the rainbow,” or preparing different-colored fruits and vegetables to get a range of vitamins and nutrients. Fresh fruits and vegetables are best, but frozen and canned produce is still a smart option.
- Lean Proteins: Prepare different types of lean protein, and allow fatty proteins (such as red meat) in moderation. Fish, seafood, and poultry are all examples of lean protein. Vegetarian options include tofu, tempeh, nuts, eggs, beans, and legumes.
- Low-Fat Dairy: Opt for low-fat dairy items — such as low-fat Greek yogurt, milk, or cottage cheese — rather than their full-fat counterparts. For senior adults who don’t consume dairy, many dairy-free alternatives, including soy milk and soy yogurt, are still low in fat.
- Whole Grains: Whole-grain bread, pasta, and cereal are a better option than plain, simple grains (such as white bread or white rice). While senior adults can enjoy staple grains, like oats and brown rice, there are many other grains to experiment with, including quinoa, bulgur, and millet.
Similarly,
there are foods that senior adults should limit, avoid, or completely eliminate
from their diet:
- Saturated Fat: Saturated fats can be found in processed foods, red meat, butter, and many desserts. Some fats, like monounsaturated and polyunsaturated fat, are healthy, but saturated fats can negatively impact health. While they can be consumed in moderation, it’s better to look for healthier sources of fat, such as avocados, fatty fish (including salmon and trout), and olive oil.
- Sodium: Sodium can be found in many pre-packaged and processed foods, canned goods, and frozen meals. Consuming too much sodium can also have negative health effects. Fresh and whole foods often contain less sodium and are a better option.
- Sugar: Sugar can be found in many different types of foods and drinks. Like saturated fat and sodium, eating a lot of sugar can potentially negatively impact physical and mental health.
Simply put, guide your loved one or patient toward whole foods that are nutritionally dense, and help them limit or avoid heavily processed or prepackaged foods.
Foods that May Benefit Those With Memory Disorders
There is a strong link between the food you eat and your cognitive functioning. While certain foods can have a negative impact on brain health, others can have a positive effect. Some foods have even been shown to reduce the risk of developing Alzheimer’s disease. While researchers continually discover new ways to treat Alzheimer’s, preventing memory loss is crucial — especially when making simple dietary changes can have such big health benefits.
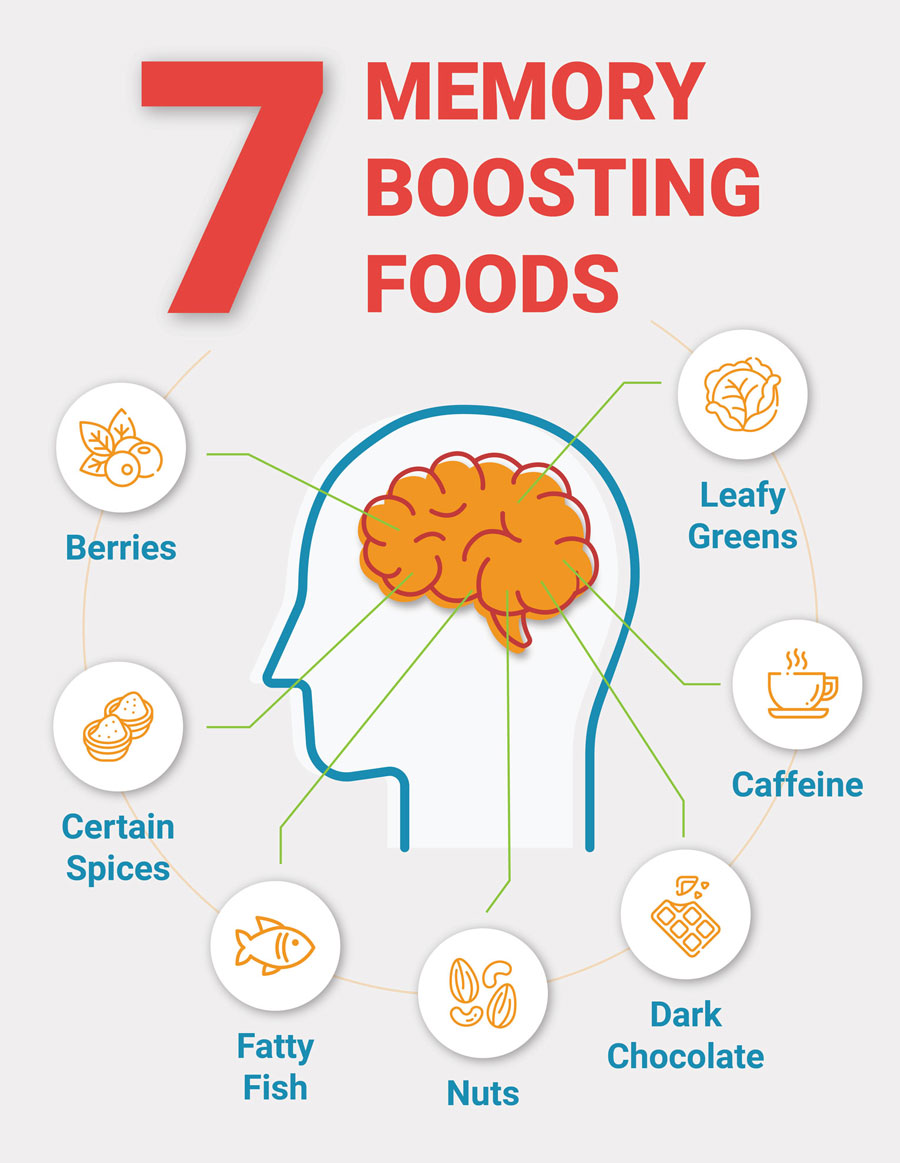
Whether your loved one is looking to lessen their risk of developing a memory disorder or prevent their disorder from worsening, encourage them to integrate the following foods in their diet:
- Berries: Blueberries and strawberries contain memory-boosting antioxidants and may slow cognitive decline. Blueberries, in particular, appear to improve memory and overall cognitive functioning in senior adults.
- Certain Spices: Some spices have been linked to improved brain health. Cinnamon has been shown to boost memory and may reduce the buildup of brain proteins that can contribute to Alzheimer’s disease. Additionally, turmeric contains a compound called curcumin, which can enhance cognitive functioning and brain health.
- Caffeine: Consuming caffeine can boost and support memory. Coffee has also been shown to slow the progression of memory impairment and may prevent memory loss from developing into dementia. For maximum effect, it’s best to stick to coffee and tea, rather than sugary soft or energy drinks.
- Dark Chocolate: Dark chocolate is full of flavonoids, antioxidant-rich compounds that are thought to decrease the risk of developing Alzheimer’s and dementia. Dark chocolate has also been linked to boosted cognitive functioning and reduced rates of cognitive decline.
- Fatty Fish: Salmon, tuna, sardines, and trout are full of omega-3 fatty acids. Not only are omega-3 fatty acids good for overall brain health, but they may also decrease the risk of age-related cognitive decline and the development of dementia and Alzheimer’s.
- Leafy Greens: Kale, spinach, swiss chard, bok choy, and other leafy green vegetables are rich with essential vitamins and minerals. One study discovered that eating one serving of leafy greens per day could slow age-related cognitive decline in senior adults. They are particularly rich with folate or folic acid, a high intake of which could further reduce the risk of developing Alzheimer’s.
- Nuts: Nut consumption has been linked to improved cognition for people of all ages. Walnuts, in particular, are thought to boost memory, and may even improve the memory of individuals who already have Alzheimer’s disease.
However, these aren’t the only foods that can impact memory, and there are multiple diets well-suited to senior adults who are looking to support brain health.
Foods That May Boost NAD+
Nicotinamide adenine dinucleotide (NAD+) is a helper molecule in the human body that plays a crucial role in many biological processes, ranging from repairing DNA to converting food into energy. It is essential for human life, but NAD+ levels naturally decline as humans age. It’s thought that boosting NAD+ levels could alleviate symptoms of memory loss disorders, increase overall cognitive functioning, and protect brain health.
Nicotinamide mononucleotide (NMN) and nicotinamide riboside (NR) can help with raising NAD+ levels. They are both NAD+ precursors; the body can use NMN and NR and convert them into NAD+. By increasing the intake of foods that are rich in NMN and NR, you may be able to boost anti-aging NAD+ levels.
Common NAD+ boosting foods include:
- Fatty Fish: Consuming fatty fish, including tuna and salmon, has been linked to increased NAD+ production.
- Green Vegetables: NMN has been found in a variety of green vegetables, including avocado, broccoli, cabbage, cucumbers, and edamame.
- Milk: Cow’s milk contains NR, and it may be present in other dairy products.
- Yeast: Researchers have discovered that yeast is an abundant source of NR.
Many of these foods have other benefits for senior adults and can be a regular part of a healthy diet. Some NAD+ boosting foods are even staples in other brain-boosting diets, including DASH, the Mediterranean, and MIND diets.
The DASH Diet
The Dietary Approaches to Stop Hypertension (DASH) diet is designed to prevent and treat high blood pressure. It focuses on reducing sodium intake, while increasing intake of nutrient-dense foods. Because senior adults with hypertension are more likely to develop markers of Alzheimer’s, some professionals speculate that controlling blood pressure could reduce the risk of developing this disease. Further, researchers believe adhering to the DASH diet can slow rates of cognitive decline in senior adults.
The DASH diet encourages participants to eat:
- More fruits and vegetables;
- Whole grains instead of refined grains;
- Small amounts of low-fat dairy products or dairy alternatives;
- Small amounts of lean meats, including poultry and fish;
- More nuts, seeds, and legumes;
- Minor amounts of healthy fats;
- And minor amounts of low-fat or fat-free sweets.
If your loved one starts the DASH diet, they still need to eat salt, as sodium is a necessary nutrient for maintaining health. Instead of eliminating salt, think of the DASH diet as a way to help them consume sodium more mindfully and increase the amount of whole, nutrient-rich foods in their diet.
The Mediterranean Diet
The
Mediterranean diet is based on the foods and cooking methods of countries near
the Mediterranean Sea, including Italy and Greece. While it was originally
designed to promote heart health, it has since been found to have a variety of
health benefits — including benefits for the brain and cognition. Adhering to
the Mediterranean diet could decrease the risk of
cognitive impairment and even prevent typical memory loss from developing into
Alzheimer’s or dementia.
The Mediterranean diet involves eating:
- More fruits and vegetables;
- Whole grains, rather than simple or refined carbohydrates;
- Healthy fats, such as avocado and olive oil;
- Dairy products, on occasion;
- Lean proteins, including poultry, seafood and fish, beans, and eggs;
- Less red meat.
The diet is primarily plant-based, though participants can eat seafood and meat. On this diet, your loved one should also avoid highly processed foods, added sugars, and unhealthy fats. Despite these restrictions, the Mediterranean diet is highly flexible and can easily be adapted to suit your loved one’s preferences.
The MIND Diet
The
Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet was
designed specifically to delay the onset of memory loss and the development of
Alzheimer’s and dementia. It combines aspects of both the Mediterranean and the
DASH diets to help senior adults support their brain health. Researchers have
questioned the effectiveness of the MIND diet, but multiple studies have found
that it appears to reduce
age-related cognitive decline and could be an effective way to decrease the risk of
Alzheimer’s and dementia.
The MIND diet works differently from other diet plans. Rather than dictating
specific meal plans or foods to eat and avoid, the MIND diet encourages
participants to eat more of 10 foods that have been proven to benefit brain
health:
- Beans and lentils;
- Berries, especially blueberries and strawberries;
- Fish and seafood, and fatty fish when possible;
- Leafy greens;
- Olive oil;
- Nuts;
- Other vegetables;
- Wine, particularly red wine, in small amounts;
- Whole grains.
The MIND diet also outlines five foods that participants should try to eat less of, including:
- Butter and margarine;
- Cheese;
- Fried food, especially from fast-food restaurants;
- Pastries, sweets, and processed desserts;
- Red meat, including pork, beef, and lamb.
You can help your loved one or patient adapt the MIND diet to suit their needs and preferences, without completely sacrificing their favorite foods or foods not included in the diet. Even making small changes or moderately following the diet could still be beneficial for them.
Foods That Negatively Impact Memory
Among other health problems, people with less healthy diets are at a greater risk of experiencing cognitive decline, including issues with memory. “Healthy diet” may be a subjective term, but there are foods that have been linked to reduced cognitive function and memory. Foods that can negatively impact memory include:
- Alcohol: Alcoholic beverages can have short-term impacts on memory. However, one study determined that heavy alcohol consumption is a major risk factor for dementia; it was also linked to early-onset dementia.
- Aspartame: Aspartame is an artificial sweetener used to replace sugar in food and drinks, most commonly in diet sodas. One study discovered that individuals who drink diet soda daily are three times more likely to develop dementia.
- Refined Carbohydrates: Consuming refined carbohydrates, such as white flour, has been continually linked to poor memory and other cognitive declines. In one study, researchers found that senior adults who consumed more than half of their calories in the form of carbohydrates were almost twice as likely to have cognitive impairments or develop dementia.
- Sugar: One study found that high-sugar diets can result in the development of health conditions — such as type II diabetes — that put senior adults at a greater risk of developing Alzheimer’s. Another determined that higher glucose levels could be a risk factor for dementia, whether or not someone has diabetes.
- Trans Fats: Trans fats can be found naturally in certain dairy products, but artificial trans fats are a major cause for concern. Multiple studies have found that eating trans fats can lower cognitive functioning, negatively impact brain health, and increase the risk of Alzheimer’s and dementia.
Many of these foods are difficult to eliminate from a patient or loved one’s diet entirely, but in order to promote brain health, it’s best to avoid them as much as possible.
Dietary Supplements for Seniors
In
addition to a nutritionally rich diet, senior adults may need to take
supplements to ensure they are getting all of the nutrients they need to
maintain health. According to one poll, 68% of seniors take
supplements regularly, while one study found that almost one-third of seniors
take at least four dietary supplements. However, it’s important to be cautious
when incorporating supplements into a senior adult’s health regimen.
If possible, it’s best to get nutrients from food. Supplements can be used to
fill any nutritional gaps, but they should never replace real food. If your
patient or loved one is struggling to eat or missing out on key nutrients,
supplements can be a helpful addition to their diet. Supplements can interact
with medications and impact the body in unexpected ways, so you should always
talk to a doctor or medical professional before giving any to a senior adult.
They can also help you find the appropriate supplement for your loved one’s
specific needs.
There are many different types of supplements that can assist senior adults
with memory, boost cognitive functioning, and support brain health, including:
Vitamins & Minerals
Taking vitamin or mineral supplements can help your patient or loved one get the essential nutrients they need, if their physician has indicated that they have a deficiency. It is important to consult a physician before beginning any vitamin supplementation, as it is possible to intake excessive amounts of vitamins and cause negative side-effects. The following vitamin and mineral supplements could be helpful for senior adults with memory impairments who have a deficiency:
- Vitamin A: Vitamin A plays an important role in vision, immunity, and reproduction, and cognitive functioning. Some research indicates that vitamin A could be useful for combating age-related cognitive decline, but further study is necessary to fully understand its benefits.
- B Vitamins: Certain B vitamins — including B6, B9, and B12 — are associated with maintaining brain health. One study suggests that taking vitamin B9 and B12 supplements, in particular, could boost brain functioning.
- Vitamin D: Vitamin D is an essential nutrient for brain health. Individuals with vitamin D deficiency could be at a greater risk of developing Alzheimer’s and dementia. Taking a vitamin D supplement could help ensure your patient does not have a deficiency. Further, one study found that taking more than the daily recommended dose of vitamin D could positively impact memory in senior women.
- Vitamin E: Vitamin E acts as an antioxidant and protects against oxidative stress. It is particularly important for senior adults to get adequate vitamin E to support healthy brain function. In addition, researchers discovered that taking high amounts of vitamin E could benefit individuals who already have Alzheimer’s or dementia.
- Iron: Though it is a vital mineral for many physical and mental processes, iron deficiency is the most common nutrient deficiency in the world. Iron deficiency can directly harm memory; however, taking an iron supplement can reverse those effects.
- Magnesium: Magnesium is a mineral that supports many different bodily processes, including cognitive performance. Magnesium deficiency has been linked to the progression of Alzheimer’s and dementia; senior adults with magnesium deficiency may greatly benefit from a supplement. Further, certain magnesium supplements could help boost memory in healthy children and adults.
Remember, these supplements are meant to augment or support your loved one’s diet, not replace it. You cannot “boost” the immune system or restore cognitive function just by taking higher doses of essential vitamins; excessive supplementation can run the risk of vitamin toxicity. If possible, it’s always best to prevent memory loss through diets that have been proven to be effective for individuals with memory impairments, and be sure to consult a physician before beginning any vitamin regimen.
Fish Oil
Fish
oil is extracted from fatty and oily fish, including mackerel, salmon, and
sardines. It contains omega-3 fatty acids. Taking a fish oil supplement can
help individuals get the nutritional benefits of omega-3 fatty acids if they
are unable to eat fatty fish.
Fish oil has a variety of purported benefits, but it could be helpful in
promoting brain health. Many studies have determined that fish oil supplementation is not as beneficial
as eating fish, but some senior adults have found success when using it to
improve memory. Another study found that while fish oil was ineffective for
moderate and severe memory loss, it did have positive impacts on subjects with mild
Alzheimer’s disease.
Glucosamine
Glucosamine is a natural sugar found in human cartilage. Glucosamine supplements are often used to promote joint health, but it could also be useful for supporting cognitive functioning. One study found that glucosamine helped improve spatial learning and memory in rats and suggests that it could have uses in preventing or treating neurodegenerative diseases like Alzheimer’s.
Herbs and Botanicals
Many herbs and plants have medicinal properties that may be beneficial for improving memory, increasing cognitive function, and maintaining brain health. Some herbs that could be particularly useful for memory impairments include:
- Echinacea: Commonly known as coneflower, echinacea has long been used as an herbal remedy. Its usefulness as a treatment for neurological disorders is still unclear, but one promising study found that it helped reduce memory loss caused by inflammation in mice.
- Ginkgo Biloba: The leaves of theGinkgo Biloba tree have been used as an herbal remedy for mental clarity, memory improvement, and boosted brain functionality. Recent studies about its efficacy have been mixed, though some research suggests Ginkgo could benefit individuals with mild cognitive impairment or early-stage Alzheimer’s.
- Gotu Kola: Gotu Kola is a flowering plant commonly called “the herb of longevity.” Not only is it reportedly used to boost cognitive functioning, but it could have a future as an Alzheimer’s treatment. In one small study, Gotu Kola appeared to have a positive effect on mice with Alzheimer’s disease.
- Lemon Balm: An herb from the mint family, lemon balm has many purported mental health benefits. Though research is somewhat limited, multiple studies have determined that lemon balm may improve memory and could be useful in managing mild cases of Alzheimer’s disease.
- Sage: Sage is frequently used as an herb in cooking, but it may have cognitive-enhancing properties, suggesting its benefits for individuals with memory impairment. However, further research is necessary to understand how sage can positively impact brain health.
- St. John’s Wort: St. John’s wort is frequently used to treat mental health issues, including anxiety and depression, but it may have benefits for brain health and cognition. In a study on rats, it was found to prevent certain memory impairments, indicating that it could be similarly useful for humans.
Herbs and botanicals may be natural, but they can still have profound and powerful impacts on the body. Some, such as St. John’s wort, can render medications ineffective or cause severe side effects. Always consult with a medical professional before suggesting any herbal supplements to a senior adult.
Anti-Aging Supplements
While there are many false claims of anti-aging supplements, some compounds may be an effective way to reduce the effects that aging has on cognition and brain health:
- Acetyl-L-Carnitine (ALCAR): ALCAR is a naturally-occurring amino acid that produces energy in cells. A growing body of research suggests that ALCAR can improve brain function in individuals with neurological conditions, as well as in healthy individuals. One study discovered that it could even reverse the decline and effects of Alzheimer’s disease when taken daily.
- Coenzyme Q-10 (CoQ10): CoQ10 is a naturally-occurring compound in the human body that helps create energy in cells. Because it can also act as an antioxidant, CoQ10 may protect the brain from oxidative stress, which is often a precursor to Alzheimer’s disease. Simply put, CoQ10 has potential as a treatment for Alzheimer’s and other cognitive disorders. Because senior adults have lower levels of CoQ10, taking a supplement could slow cognitive decline and improve the overall quality of life.
- NMN: Though it’s present in certain foods, NMN can have benefits when taken as a supplement. It may be particularly useful for senior adults who are looking to boost NAD+ levels or don’t get enough NMN in their diets. Increased intake of NMN, in particular, has been linked to improved cognitive function and may even have value as a treatment for Alzheimer’s disease.
It’s worth noting that, while these compounds do have promising benefits for cognitive functioning, the research is still in its infancy. Further study is necessary to determine exactly how beneficial these anti-aging supplements can be for memory-impaired senior adults.
Additional Resources for Seniors, Families, and Caregivers
As an aging adult, you should always talk to your primary care provider before making any changes to your diet or before starting a care plan. However, if you’re looking for more information, there are plenty of resources available that can offer additional guidance and support for you, your family members, and your caregivers.
Memory Disorder Resources
Consult the following resources for more information on how to live with and manage a memory disorder:
- Alzheimer’s Association (AA): AA is working to put a stop to Alzheimer’s, dementia, and other memory loss conditions. In addition to researching these conditions, they also help patients find high-quality care and support.
- Alzheimer’s Association 24/7 Helpline: The AA helpline is available all times of the day and night, every single day of the year. You can use this confidential helpline to connect with clinicians and specialists if you need assistance or support.
- BrightFocus Foundation: This nonprofit organization conducts and supports research on memory loss and vision disorders. They also provide factual and informative resources explaining the science behind the conditions they study.
- Living With Memory Loss: A Basic Guide: This handbook was put together by the team at the University of Washington’s Memory Brain Wellness Center. From understanding your diagnosis to making future plans, it will guide you, step by step, through life with a memory disorder.
- Memory Loss and Forgetfulness: This page from the National Institute on Aging contains essential information that can help you understand any memory issues you’re experiencing, as well as how you can get help.
- Understanding Memory Loss: Put together by the National Institute on Aging, this booklet explains the difference between memory loss and forgetfulness, provides basic facts about Alzheimer’s and dementia, and offers guidance so you can get the help you need.
Caregiver and Family Resources
To help support an aging family member or someone with a memory disorder, please peruse the following resources:
- Alzheimer’s Association Glossary: This glossary from the Alzheimer’s Association defines many of the common terms related to memory loss that caregivers and family members need to be familiar with.
- Alzheimer’s Family Center: Based in Orange County, California, this organization provides myriad online resources to help, assist, and support caregivers and family members of people with memory impairments — regardless of their physical location.
- Dementia Friendly America (DFA): DFA is an advocacy and support organization that connects people living with dementia, and their caregivers, to the helpful resources. They are a national network that allows caregivers to connect with each other. Additionally, they offer a variety of toolkits and resources to support local-level advocacy efforts.
- Family Caregiver Alliance: This organization works to assist and educate the caregivers and family members of individuals with chronic health conditions. They offer resources about education, care planning, and ongoing support to improve the quality of life for caregivers and the people they care for.
- Family Caregiver Toolbox: Put together by the Caregiver Action Network, this page offers a wide range of helpful tools and information for family caregivers. It is especially useful if you’re new to caregiving.
- Getting Help with Alzheimer’s Caregiving: This resource page from the National Institute on Aging provides information to memory loss caregivers on a variety of important topics, including additional care support, meal services, and hospice care.
- Memory Cafe Directory: In an effort to combat social isolation,memory cafes connect people with memory impairments and their caregivers with other people who are going through similar experiences. This directory helps you to find memory cafes in your community.

