Stanford Study Shows Small Molecule Treatment Restores Nerve Function and Enhances Strength
Sanford Burnham Prebys and Stanford University demonstrate that blocking an enzyme (15-PDGH) can improve neuromuscular connectivity and muscle strength during injury, disease, and aging.
Highlights:
- In mice, levels of an enzyme called 15-PDGH significantly increase in muscle following nerve damage.
- Blocking 15-PGDH promoted regeneration of motor neurons and accelerated recovery.
- 15-PGDH is a marker of muscles affected by neurogenic myopathies in human subjects, supporting the therapeutic potential of this treatment.
Researchers from Stanford University School of Medicine and Sanford Burnham Prebys found an enzyme that might be key to helping keep nerves and muscles healthy as people age. The enzyme, 15-hydroxyprostaglandin dehydrogenase (15-PGDH), accumulates with age and is thought to be partially responsible for age-related muscle wasting. In old mice, blocking 15-PGDH made the connections between nerves and muscles stronger and sped up the healing process in the neurons that control movement. In humans with conditions affecting the nervous system and muscles, diseases like ALS and SMA, researchers found that 15-PGDH was present in muscle fibers. These results, which were published in Science Translational Medicine, suggest that blocking 15-PGDH using a drug may be a way to help regenerate their connection with the nervous system and get stronger after losing connection due to illness, injury, or getting older.
As nerves age, muscles can wither away
Whether you are walking, swimming, or lifting weights, your muscles depend on the nervous system to work properly. Your brain and spine are where nerve impulses originate, they travel along motor neurons (long cells connecting the spine to all muscles in the body) until they reach the muscles. This area where the motor neuron touches the muscle is called the neuromuscular junction (NMJ) and is incredibly important because this is where the signal is sent to the muscle of interest to get it to flex.
When NMJs begin to deteriorate, the signals sent from our nervous systems to our muscles begin to weaken. This process is called denervation and can happen after serious injury, because of neuromuscular wasting diseases like ALS or SMA, or more generally as we age.
Blocking 15-PGDH enhances muscle recovery after nerve damage
In this study, scientists from Helen Blau and Hannes Vogel’s labs tried to figure out what parts of the denervation process might be important in order to target them to help motor neurons grow back. To do so, the researchers crushed the sciatic nerve—the nerve that extends from the lower back through your hips and buttocks and down each leg—in mice. This nerve damage results in a significant increase in muscle 15-PGDH levels, significant denervation of the muscles of the hind legs, and decreases in muscle strength.
Interestingly, mice that were treated with a drug that inhibited 15-PGDH after receiving nerve damage saw faster regeneration of motor neurons and improved formation of NMJ connections, leading to faster recovery of muscle strength.
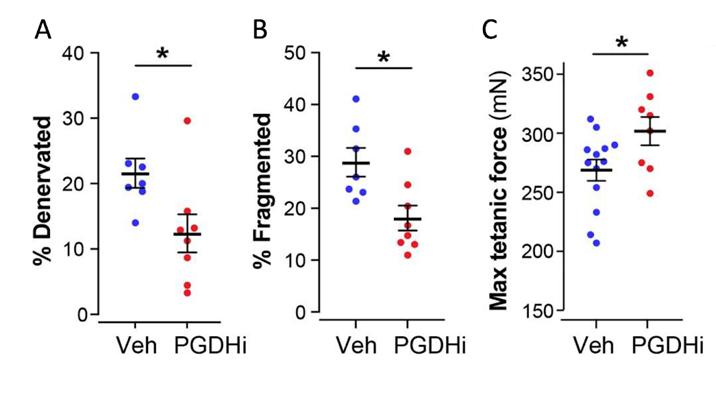
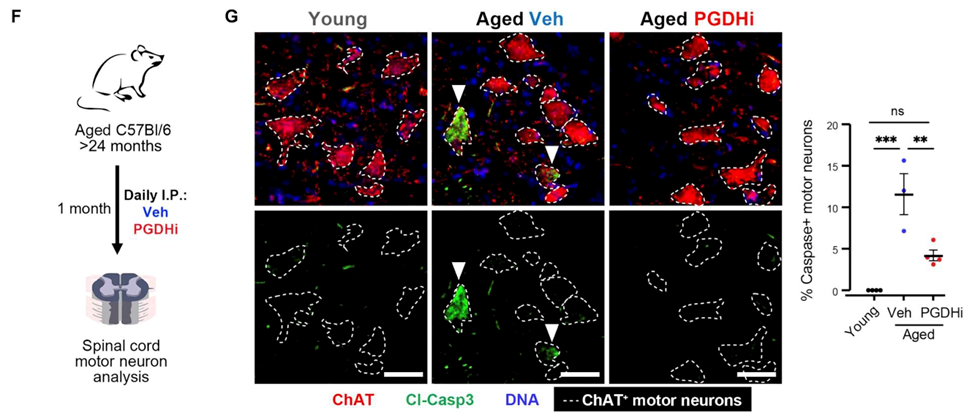
The 15-PGDH inhibitor increased the viability of motor neurons and restored neuromuscular junctions and function in old mice whose muscles had been denervated for a long time. These presynaptic changes synergized with previously reported muscle tissue remodeling to result in a marked increase in the strength of aged muscles.
To test whether 15-PGDH was associated with decline in nerve/muscle function in humans, researchers analyzed muscle biopsies from patients with neurogenic myopathies. Their analysis revealed there as a buildup of 15-PGDH proteins in this patient population. But when they analyzed muscle biopsies from healthy patients they were not able to detect 15-PGDH. These results suggest that 15-PGDH might have something to do with how these diseases progress.
The promise of 15-PGDH inhibitors
The enzyme 15-PGDH is a really interesting target because it has been shown to be key to halting tissue stem cell activity and, thus, can block tissue repair and regeneration as the result of injury and, perhaps, even aging. Along these lines, blocking 15-PGDH has been shown to accelerate regeneration and repair in multiple mouse models of organ diseases. These therapeutic effects range from accelerating mucosal healing in colitis, to markedly accelerating recovery of the hematopoietic system (blood and immune cells) after bone marrow transplantation, to enabling lung recovery from scarring.
In fact, previous research from the same lab had shown that 15-PGDH is increased in aged muscles and drives age-related muscle atrophy and that inhibition of 15-PGDH by a small molecule improved muscle health and increased strength. So, what’s really novel about this paper is that in addition its known function in improving muscle health and strength, the effects there spread to the connecting serves, which stretches the number of conditions that 15-PGDH inhibitors can affect.
The conclusion of this research is that blocking 15-PGDH might be an easy and useful way to help muscles and nerves recover after nerve damage. This strategy benefits from its complementary effects on muscle and motor neurons to restore their connectivity. Promoting motor axon and NMJ regeneration could potentially be applied to conditions where muscle denervation leads to the loss of strength and function, including acute trauma, nerve compression injuries, chronic neurodegenerative disorders, and motor neuron diseases like ALS and SMA.
Model: Sciatic nerve crush in adult mice; 26 month old mice
Dosage: Intraperitoneal injection of 15-PGDH inhibitor (SW033291) or control once daily for 14 days

