Study Shows NMN Enhances Stem Cell Vesicle Therapy for Heart Attack Damage
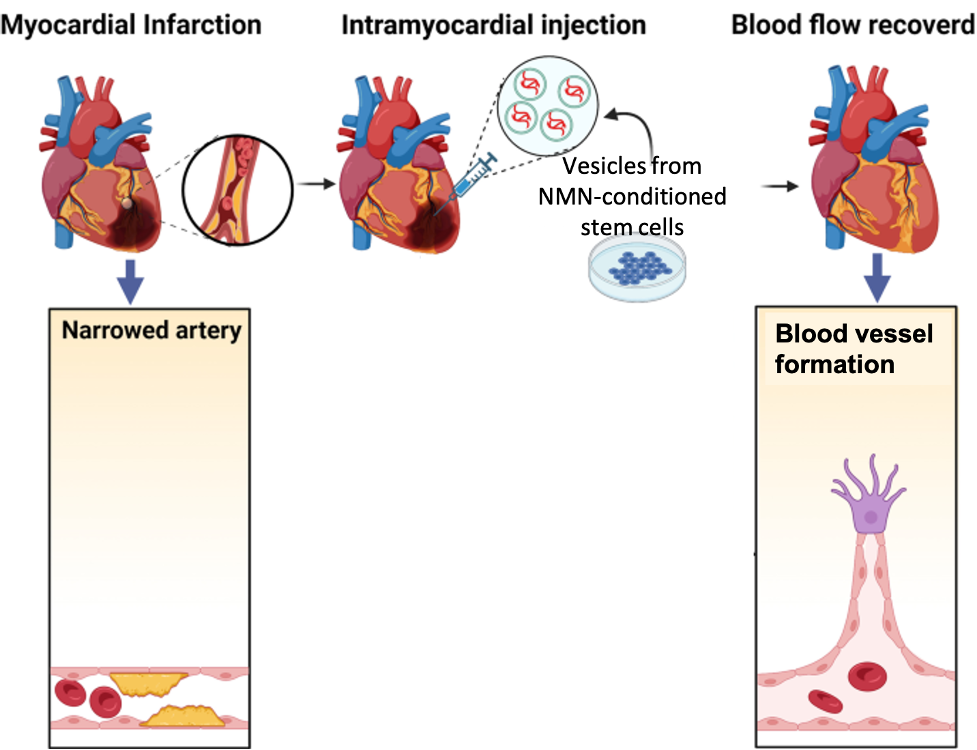
Vesicles secreted from NMN-treated stem cells improve heart function while promoting blood vessel formation and reducing tissue damage after myocardial infarction (heart attack) in rats.
Highlights:
- Vesicles secreted from stem cells treated with NMN (N-Vs) improve heart function in rats following heart attack.
- N-Vs promote blood vessel formation, namely small arteries and capillaries, after heart attack.
- Heart tissue recovery is enhanced by N-Vs following heart attack, as shown by reduced heart cell death and tissue scarring.
Heart attacks account for 80% of deaths resulting from heart disease, the leading cause of death worldwide. Heart attacks are caused by cell oxygen deprivation due to blood vessel blockage, leading to fatal levels of heart tissue damage. In an effort to prevent death, it is critical to restore blood flow and repair this tissue damage as soon as possible. Current options include surgery or medications like aspirin.
Now, Pu and colleagues from The First Affiliated Hospital of Nanjing Medical University in China report in Stem Cell Reviews and Reports that vesicles secreted from stem cells treated with NMN (N-Vs) may reduce heart damage and dysfunction after heart attack. Namely, in a heart attack rat model, N-V injections improve heart function, increase blood vessel formation, and reduce tissue damage. These results suggest that stem cell-derived vesicles, especially when conditioned with NMN, can reduce heart damage from heart attack.
NMN Enhances Stem Cell Vesicle Heart Repair
Recent studies have indicated that stem cells (mesenchymal stem cells) secrete membrane-bound sacs called extracellular vesicles that are filled with potentially therapeutic molecules. Like stem cells, these vesicles possess curative properties. They also have advantages over stem cells, including a lack of immune system rejection and tumor induction. When conditioned with various stimuli, stem cell vesicle content can change, influencing their biological effect.
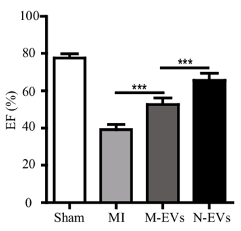
Pu and colleagues surgically induced coronary artery blockage in rats to cause heart tissue damage and simulate a heart attack. They then injected the rats at the border of the tissue damage with untreated stem cell vesicles or NMN-treated stem cell vesicles. After four weeks, they found that untreated vesicles increased left ventricular ejection fraction — the fraction of blood pumped by the heart. Moreover, N-Vs increased the ejection fraction further, indicating enhancement of heart function repair.
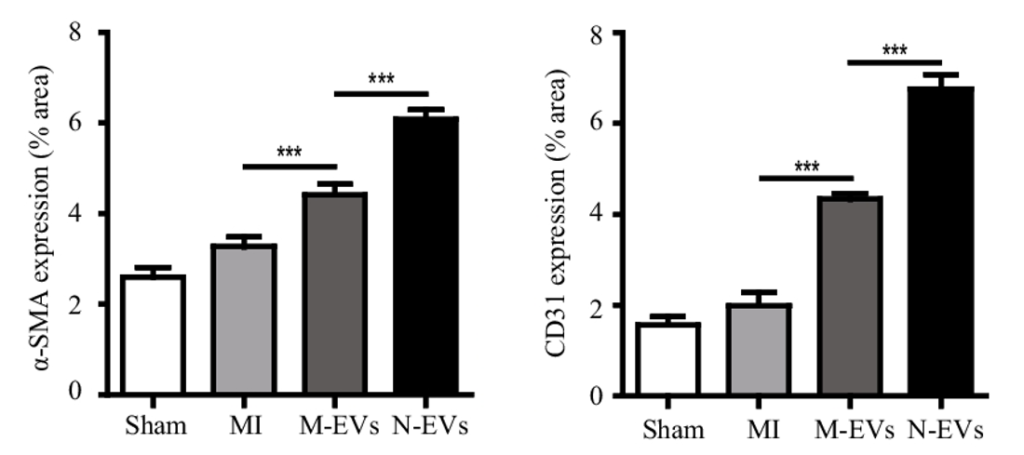
The pumping-action of the heart is most efficient when blood flow, mediated by blood vessels, is optimal. Pu and colleagues found that untreated stem cell vesicles increased small artery and capillary density in the heart tissue of rats following heart attack. Additionally, artery and capillary blood vessel density were further increased by N-Vs. These findings demonstrate that NMN enhances vesicle-mediated blood vessel formation, which should increase blood flow.
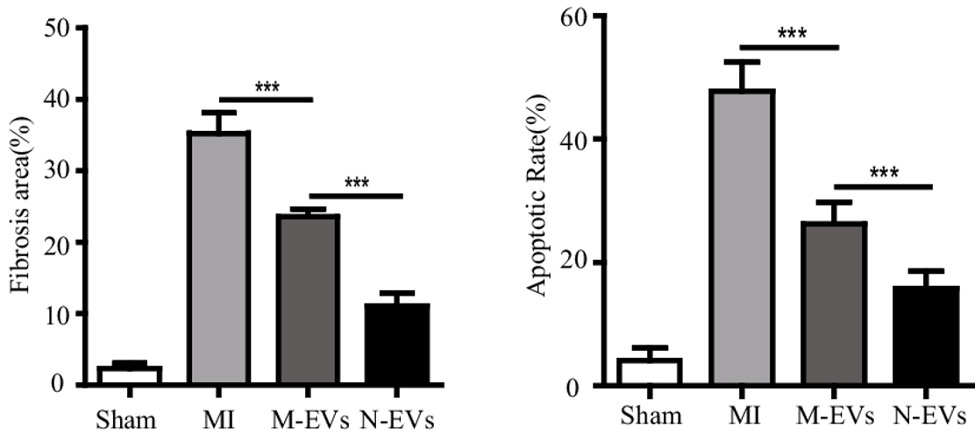
New blood vessel formation contributes to reduced tissue scarring —fibrosis — and cell death in cardiac tissue damaged by heart attack. Pu and colleagues found that fibrosis decreased in response to untreated stem cell vesicles, and that fibrosis decreased more with N-Vs. Furthermore, programmed cell death — apoptosis — was reduced by normal vesicle injections and again reduced by N-V exposure. These findings indicate that NMN enhances stem cell vesicle-mediated cardiac tissue repair.
“Our study demonstrated that extracellular vesicles derived from [stem cells] could improve cardiac function by promoting [blood vessel formation], promoting proliferation, inhibiting apoptosis, reducing fibrosis, and improving cardiac function, which is further enhanced after NMN treatment,” say the authors.
A Future of NAD+-Enhanced Cell-Free Therapy
Stem cells have been applied to the treatment of many diseases, including neurological disease, respiratory disease, fracture healing, and cardiovascular disease. As increasing evidence shows that stem cell vesicles have similar effects, as well as advantages, we may see a shift in research towards so-called cell-free therapy, which is essentially stem cell therapy without the stem cells. Indeed, cell-free stem cell vesicles have been shown to alleviate arthritis and other age-related effects in rodents.
Pu and colleagues take cell-free therapy a step further by showing that NMN, an NAD+ booster, can enhance the therapeutic effects of stem cell-derived vesicles. Previous studies have shown that NMN rejuvenates stem cells, which could explain its enhancement effects. If cell-free therapy proves to be viable, it’s possible that NAD+ boosters or other stem cell rejuvenating compounds could promote the fitness of stem cells and their vesicles to enhance said therapy.

